What Is Pudendal Neuralgia in Females?

Pudendal neuralgia (PN) is a painful condition caused by the irritation or compression of the pudendal nerve, which is responsible for sensation and function in the pelvic area. Common causes include prolonged sitting, activities like cycling, and pelvic trauma.
In women, PN can occur due to childbirth and hormonal changes. Symptoms may include pelvic pain, numbness, and difficulties with bladder and bowel control. Women can also experience pain during intercourse, increased pelvic floor tenderness, and changes in the discomfort associated with menstruation.
At Centeno-Schultz Clinic, we understand how these issues can impact your daily life, affecting physical and emotional well-being. Our approach uses tailored treatment plans that prioritize non-invasive, regenerative therapies to target the root cause of pain, helping you regain your quality of life without the risks and recovery times associated with medications or surgery.
Understanding Pudendal Neuralgia Pain
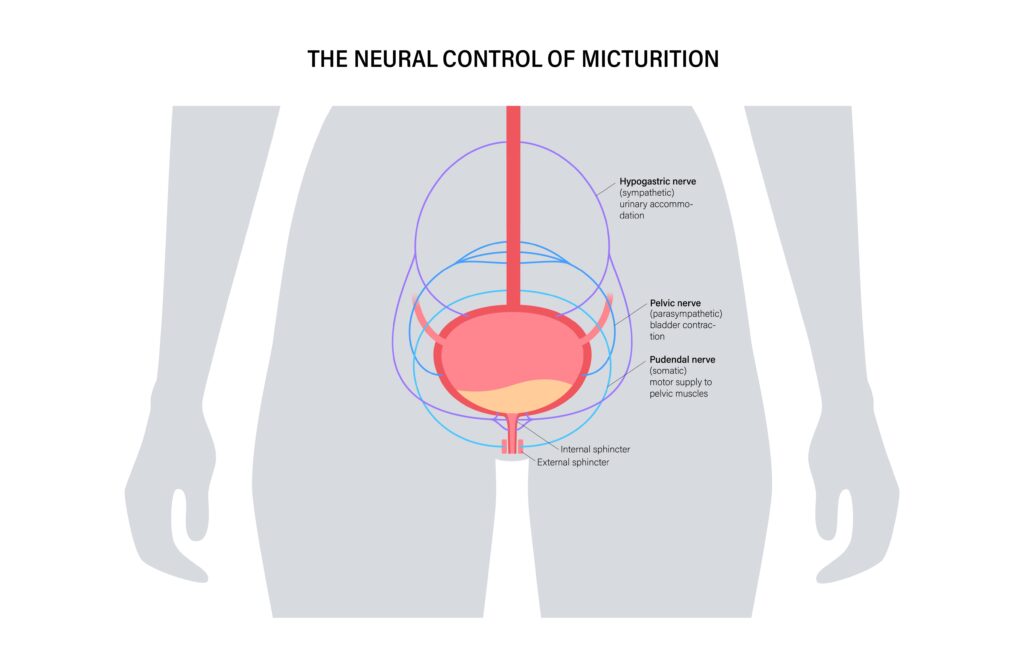
PN is a condition that affects the pudendal nerve, which is important for feeling and movement in the pelvic area. The pudendal nerve originates from the spinal nerves in the lower back, between the second and fourth sacral vertebrae (S2-S4). It then travels through a part of the pelvis called the pudendal canal and reaches areas like the genitals, anus, and perineum.
The main functions of the pudendal nerve are:
- Sensation: This nerve provides feeling to the genitals, anus, and the perineum, allowing for sensations like touch.
- Motor control: It controls the muscles involved with functions such as urination and bowel movements.
PN happens when your pudendal nerve is squeezed or irritated. This can occur from sitting too long, frequent cycling, or after pelvic surgery or childbirth, which might stretch the nerve.
You might feel sharp, burning pain, numbness, more sensitivity, and you could have trouble with bladder or bowel control, or experience sexual dysfunction. These symptoms can impact your daily activities and emotional well-being, causing stress and making social interactions tough.
Additionally, this condition is often misdiagnosed, which delays treatment. This delay can lead to increased painkiller use, like opioids, that don’t address the root cause of pain and carry risks like addiction.
Does the Condition Affect Women Differently Than Men?
Due to anatomical differences, PN can have different causes and symptoms in females. For women, childbirth can stretch or compress the pudendal nerve. Hormonal changes throughout a woman’s life can also influence the severity and frequency of symptoms.
Since the pudendal nerve also plays a role in sexual function, females can experience pain during sex and chronic pain around the vulva. Men, on the other hand, might have issues such as erectile dysfunction. While both men and women can experience similar types of pain and discomfort, the specific symptoms can differ.
Areas Affected by Pudendal Neuralgia in Women
PN can cause discomfort in several areas of the pelvic region. The primary areas affected include:
- External genitalia: You might experience pain, burning, or numbness in the vulva, clitoris, or surrounding skin. These sensations can range from mild to severe and may worsen with activities like sitting or wearing tight clothing, which can further compress the pudendal nerve.
- Perineum: This is the area between the vagina and the anus. It is innervated by the pudendal nerve, and when this nerve is irritated or compressed, it can lead to tenderness, swelling, or increased sensitivity. Prolonged sitting can worsen this symptom.
- Anal and rectal region: Pain may be felt around the anus or even deep inside the rectum. This can make bowel movements uncomfortable or painful.
- Adjacent pelvic floor structures: The pudendal nerve also provides motor function to the muscles that support the pelvic organs. When the nerve is compressed, it can lead to feelings of heaviness or pressure in the pelvis, which contribute to bladder or bowel control problems.
Factors That May Lead To This Condition
PN can arise from several factors that put stress or pressure on the pudendal nerve. Some, such as prolonged sitting, can affect both men and women, while others, such as childbirth, are gender specific.
Understanding these factors can help identify risks, preventive measures, and effective interventions.
Childbirth
During childbirth, the pudendal nerve may be stretched or compressed due to the baby’s descent through the birth canal. This pressure can cause nerve irritation or damage, leading to PN, especially if the delivery involves prolonged labor or the use of forceps.
Research on the impact of childbirth on the pudendal nerve is limited. A 2014 study reports that nerve damage occurs in 32% of all vaginal deliveries. However, 8 in 10 cases resolve without medical intervention within six weeks.
Additionally, 2023 research shows pelvic floor dysfunction affects one in three women, often starting from childbirth-related nerve injury. Vaginal births, especially those requiring the assistance of specific instruments, are more likely to lead to nerve trauma. Cesarean sections were less likely to cause this type of nerve involvement.
Surgical Procedures
Most surgical procedures come with risks, including nerve damage. In particular, the pudendal nerve can be affected during invasive treatments like bladder or rectal surgery. Procedures involving the pelvic floor, such as hysterectomies or prolapse repairs, have a higher risk.
The nerve can become severed or stretched during surgery, altering its function. Additionally, scar tissue can form around the nerve post-surgery, which can compress it.
Prolonged Sitting
Sitting for extended periods puts undue pressure on the pudendal nerve, particularly in positions that compress the pelvis. Over time, this pressure can lead to nerve irritation or even minor damage, contributing to symptoms of PN. Activities like driving, desk jobs, and cycling increase the risk.
Pelvic Trauma
Trauma to the pelvic area can result in direct injury to the pudendal nerve. This can occur from falls, car accidents, or sports injuries where the pelvis is impacted. Traumatic injuries, including fractures and dislocations of the pelvic bones, may lead to nerve compression, stretching, or bruising in affected areas.
Radiation Therapy
Radiation therapy uses high-energy rays to destroy cancer cells, shrink tumors, and prevent cancer from spreading. It aims to spare surrounding tissues, but damage to structures such as nearby nerves, including the pudendal nerve, can happen.
This can lead to nerve inflammation or fibrosis, where scar-like tissue forms around the nerve and compresses it.
Common Symptoms of PN to Look Out For
The pudendal nerve is responsible for providing motor and sensory function to the pelvis. Compression or damage to this nerve can disrupt the transmission of signals from and to the brain, resulting in pain, numbness, and dysfunction. Common symptoms include:
Pelvic Pain
Compression of the pudendal nerve results in abnormal pain signaling, which leads to chronic pain and increased sensitivity. For instance, stimuli that should not be painful, such as light touch, are experienced as painful.
This pain is often sharp, burning, or stabbing and can be localized in the lower pelvis, near the genitals, or around the perineum. Activities that place increased pressure on the nerve, like sitting or biking, often worsen this symptom.
Urinary Issues
The pudendal nerve plays a critical role in controlling bladder function. When compressed or damaged, you might experience symptoms such as an urgent need to urinate or difficulty starting urination.
These issues occur because nerve compression can disrupt the signals that help manage the bladder sphincter, leading to miscommunication between the brain and bladder.
Bowel Dysfunction
PN can also cause difficulties with bowel control when the nerve’s ability to manage the anal sphincter is compromised. The nerve’s compromised signaling can make it challenging for muscles to properly control bowel movements. This can result in symptoms like constipation or incontinence.
Sexual Dysfunction
The pudendal nerve is crucial for normal genital sensation and sexual function. Symptoms can be gender specific. Men might experience issues such as erectile dysfunction, premature ejaculation, and ejaculation pain.
In women, sexual dysfunction symptoms related to PN include:
- Persistent genital arousal disorder (PGAD): PGAD involves spontaneous, unwanted arousal that isn’t linked to sexual desire. It can be uncomfortable and affect emotional health.
- Dyspareunia: This is painful intercourse or genital pain during or after sex. It can affect emotional and sexual well-being.
- Vulvodynia: Vulvodynia is chronic vulva pain or discomfort without an obvious cause. It can be linked to nerve irritation.
These symptoms occur due to altered nerve signaling, which affects normal sensory and motor functions in the pelvic area.
Numbness or Tingling
Numbness or tingling in the pelvis, genital area, or perineum occurs when the nerve is compressed in a way that alters normal sensory transmission. You might feel a “pins and needles” sensation, similar to when a limb falls asleep, which happens when disrupted nerve signals related to sensation do not reach the brain as they should.
When to Seek Professional Help
Experiencing mild pelvic discomfort after a day of sitting or cycling is normal. However, if symptoms persist or begin to impact your daily life, they may indicate involvement of the pudendal nerve.
Here are some signs that you should contact a healthcare provider:
- Persistent pelvic pain that is ongoing or intensifies.
- Pelvic symptoms that don’t subside within a few weeks of giving birth.
- Difficulties with controlling your bladder or bowel movements.
- Any changes in sexual function or increased pain during intercourse.
- Frequent or worsening numbness or tingling in the pelvic region.
How Doctors Diagnose Pudendal Neuralgia in Women
PN is a condition that remains difficult to diagnose. This is because there is limited healthcare provider awareness, and its symptoms can be confused with those of other conditions, like sciatica.
However, a misdiagnosis can lead to complications, including worsening symptoms, reliance on medications, stress, and affected emotional health. This makes an adequate diagnosis vital to inform treatment decisions.
Common diagnostic tools used to rule out other conditions and pinpoint nerve issues include:
- Medical history and physical exam: Your healthcare provider will review your medical history, symptoms, and lifestyle factors that could contribute to pain. They will review events, such as assisted vaginal birth, that may have affected the pudendal nerve.
- Nerve blocks: A diagnostic nerve block involves administering medications to see if numbing the pudendal nerve relieves symptoms. This can confirm the diagnosis.
- Imaging techniques: MRI or CT scans provide inner views of the structures of the pelvis. They are used to identify issues such as scar tissue, tumors, and fractures that may compress the pudendal nerve.
- Electromyography (EMG): This test measures muscle responses and nerve function in the pelvic floor. It can be used to identify problems with the transmission of nerve signals.
- Pelvic ultrasound: In females, this imaging technique uses sound waves to create pictures of organs such as the uterus, ovaries, fallopian tubes, and bladder. It helps doctors detect abnormalities like cysts, fibroids, or tumors, and can also monitor pregnancies or investigate causes of pelvic pain.
Treatment Options Available for Women
PN treatment should focus on both relieving symptoms and targeting the root cause of nerve compression. In women, therapies should also address pelvic health as a whole. Common treatment options include:
Neuropathic Pain Relievers
Neuropathic pain relievers, such as gabapentin and pregabalin, may help manage nerve pain. These medications work by calming overactive nerves, reducing the intensity of pain signals sent to the brain.
Pain relievers can mask nerve pain and provide short-term symptom relief, but they typically do not address the underlying cause of nerve injury. Alternatives that also promote nerve repair include supplements such as alpha-lipoic acid (ALA), B vitamins (especially B1, B6, and B12), CoQ10 (ubiquinone), and antioxidants like N-acetylcysteine (NAC) and acetyl-L-carnitine.
Pelvic Floor Rehabilitation
Pelvic floor rehabilitation is a type of specialized physical therapy designed to strengthen and relax the pelvic muscles. It involves physician-guided exercises, poses, and stretches to support pelvic health and alleviate pressure on the pudendal nerve. This can reduce pain, restore sexual function, and improve control of bladder and bowel functions.
Pudendal Nerve Block
A pudendal nerve block involves injecting an anesthetic near the pudendal nerve to numb it temporarily. This intervention can help reduce pain. It is also often used in the diagnosis of pelvic issues to confirm the nerve as the pain source.
Transcutaneous Electrical Nerve Stimulation (TENS)
TENS therapy utilizes mild electrical impulses delivered through the skin. These impulses interfere with the transmission of pain signals between the compressed nerve and the brain, temporarily easing symptoms. The massage-like sensations also relax muscles and encourage the body to release endorphins, which are natural painkillers.
Nerve Decompression Surgery
Nerve decompression surgery may be considered when other treatments fail to provide relief. This procedure involves releasing or removing tissue that compresses the pudendal nerve to ease symptoms. This is an invasive option that carries risks, including nerve damage and infection.
Cognitive Behavioral Therapy (CBT)
CBT is not a direct treatment for the nerve itself but offers a supportive approach to managing chronic pain. Through CBT, patients learn to adjust their pain perceptions and develop healthy coping strategies.
This mental health intervention can reduce the emotional and psychological impacts of PN, helping patients manage stress and anxiety associated with living in chronic pain.
What Happens if You Don’t Address PN?
Ignoring PN can lead to several complications that may significantly affect long-term health and quality of life. Potential issues include:
- Chronic pain: Unattended, PN can result in persistent and worsening pelvic pain. This can make daily activities more challenging and lead to reliance on pain medication.
- Bowel and bladder dysfunction: Unresolved nerve irritation can cause urinary and bowel control issues. This can impact your pelvic and digestive health and cause chronic stress, embarrassment, and declining emotional health.
- Sexual dysfunction: Over time, nerve damage might lead to ongoing sexual health problems, affecting intimacy and relationships.
- Emotional and mental health impact: Chronic pain and discomfort can lead to increased stress, anxiety, and depression, which can impact overall well-being and mental health.
- Reduced mobility: Chronic pain can make social and physical activities undesirable, leading to declining mental and physical health.
How Centeno-Schultz Clinic Supports Women with Pudendal Neuralgia
At Centeno-Schultz Clinic, we understand the complexities of living with PN—from the chronic pain to the difficulty in getting diagnosed and finding adequate treatment.
Our team of specialized physicians is committed to providing comprehensive and personalized care to target the root cause of pain. Our approach starts with a thorough diagnostic process that utilizes advanced techniques like ultrasound imaging to understand the unique factors contributing to your pelvic pain. This evaluation allows us to develop targeted treatment plans that focus not only on symptom relief but also on addressing the underlying causes of your condition.
We focus on regenerative orthopedic treatments that support your own body’s ability to heal naturally, without medications or surgery. This can help you avoid the risks and lengthy recovery periods associated with traditional interventions. Additionally, this approach aims to decrease dependency on medications and offer a pathway to improved pelvic health with less downtime.
Platelet-Rich Plasma (PRP)
Take the Next Step Toward Pudendal Neuralgia Relief
If you’re experiencing symptoms of PN, early intervention can make a difference. At Centeno-Schultz Clinic, our dedicated team is ready to help you understand what is causing your pelvic pain, find relief, and reclaim your quality of life.
Explore our personalized, non-invasive treatment options through a comprehensive evaluation tailored to your unique needs. Take the next step and schedule a consultation with us today to begin your journey toward restored pelvic health.
Our Doctors

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read more