Understanding Trigeminal Neuralgia
Causes, Symptoms, Treatments, & Other Resources
Trigeminal neuralgia is a chronic pain condition characterized by sudden, sharp, electric current-like pain in the face. This is typically triggered by even mild stimulatory motion such as chewing or talking. It occurs due to irritation or compression of the trigeminal nerve, often making everyday activities intolerable for those affected.
A groundbreaking treatment option, the IGNIte procedure, has emerged as a promising solution for refractory cases of trigeminal neuralgia. This minimally invasive technique targets the trigeminal nerve with healing growth factors from your own platelets, effectively reducing nerve hyperactivity while preserving surrounding structures.
Today, let’s explore a recent case I successfully treated using the IGNIte procedure and learn why this approach succeeded where traditional treatments had failed.

A Closer Look At The Trigeminal Nerve Anatomy
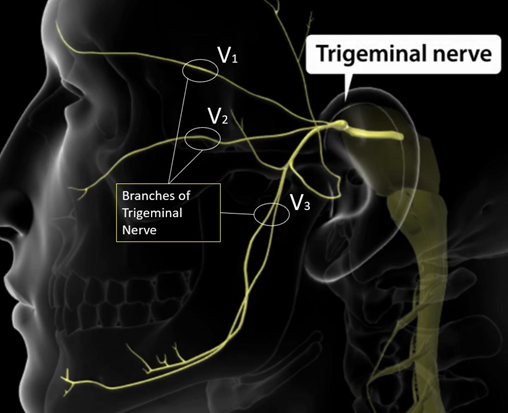
The trigeminal nerve, or cranial nerve V, originates in the brainstem and is responsible for sensory and motor innervation of the face. It has three main branches:
V1 (ophthalmic branch): Provides sensory input from the forehead, eyes, and upper nose.
V2 (maxillary branch): Relays sensory information from the cheeks, upper jaw, and nasal cavity.
V3 (mandibular branch): Unique among the branches, V3 carries both sensory and motor fibers. It supplies sensation to the lower jaw, teeth, and part of the tongue, while also powering the muscles involved in chewing and speaking.
This delicate structure is crucial for facial sensation and motor functions, making its injury or dysfunction, such as in inferior alveolar nerve injury, a significant clinical concern.
The video below highlights the V3 branch and its role in common injuries like inferior alveolar nerve damage.
What Is Trigeminal Neuralgia (TN)?
TN is a chronic pain condition affecting the trigeminal nerve, responsible for facial sensation. It is characterized by sudden, intense, and often debilitating facial pain, typically triggered by everyday activities like chewing, talking, or even light touch. TN is caused by irritation or compression of the nerve, commonly due to blood vessel contact, aging, or, less frequently, underlying conditions such as multiple sclerosis or a tumor.
Often described as one of the most painful conditions, TN can significantly impact an individual’s quality of life. While traditional treatments such as medications and surgical options aim to manage the symptoms, newer, minimally invasive procedures offer promising solutions for refractory cases.
Recognizing The Symptoms Of A TN Attack
Trigeminal neuralgia presents with distinctive symptoms that can vary in severity and frequency. Episodes are often unpredictable, making early recognition key to seeking effective treatment. The hallmark symptom is sudden, sharp facial pain, but other features may also occur, including the following.
Difficulty Chewing And Talking
Everyday actions like chewing or speaking can trigger or worsen the pain, making these essential tasks daunting.
Sharp, Stabbing Pain In The Face
The pain often feels like electric shocks and can strike without warning, primarily in the jaw, cheek, or eye area.
Localized Pain On One Side Of The Face
TN typically affects only one side of the face, corresponding to the nerve’s irritated branch.
Pain Episodes Lasting Seconds To Minutes
The attacks are brief but can occur in clusters, with multiple episodes in a day.
Burning Sensation Between Episodes
In some cases, a lingering burning or aching sensation may persist between acute pain episodes, adding to the discomfort.
Common Causes Of Trigeminal Neuralgia
Trigeminal neuralgia can result from various underlying issues that irritate or damage the trigeminal nerve. These causes include physical injury, structural compression, or procedural complications. Understanding these triggers is crucial for accurate diagnosis and targeted treatment.
Nerve Damage
Damage to the trigeminal nerve is a primary cause of TN, disrupting its normal function and causing painful episodes.
Inferior Alveolar Nerve Injury
This injury, often associated with dental procedures, is a common cause of TN affecting the V3 branch. For a detailed explanation, refer to the video above, which highlights how such injuries lead to this type of trigeminal neuralgia.
Tumors
Tumors near the trigeminal nerve can compress or damage the nerve, leading to persistent or progressive symptoms.
Physical Trauma
Head or facial trauma can injure the nerve, either directly or through swelling, resulting in neuralgia.
Anesthetic Injections
Improperly administered nerve blocks or local anesthetics can inadvertently damage the trigeminal nerve.
Endodontic Treatments
Root canal procedures, if complicated, may impact the nerve, particularly in the mandibular region.
Dental Surgical Procedures
Dental surgeries, such as extractions or implants, may inadvertently harm nearby nerve structures, potentially triggering TN.
Vascular Theory
An artery or vein may press against the trigeminal nerve near the pons or along its pathway. This can damage the protective myelin sheath and cause the nerve to malfunction, leading to sudden, intense nerve activity. Symptoms often appear in areas controlled by the V2 (middle face) or V3 (lower face) branches of the nerve.
When Do You Need To Seek Medical Help?
It’s essential to seek medical attention for trigeminal neuralgia to obtain a proper diagnosis and personalized treatment plan. Early intervention can improve outcomes and reduce the impact on daily life. Prompt medical evaluation is crucial if you experience:
- Frequent or persistent facial pain that interferes with daily activities.
- Pain that no longer responds to typical medications or becomes refractory to treatment.
- Pain that radiates or spreads beyond the usual trigeminal nerve distribution.
How Trigeminal Neuralgia Is Accurately Diagnosed
Accurately diagnosing trigeminal neuralgia involves a combination of a thorough medical history, clinical examination, and advanced imaging techniques.
- Medical history and physical exam: A detailed review of symptoms helps identify patterns of pain characteristic of TN, such as triggers, duration, and localization.
- Neurological exam: Tests focus on assessing facial sensation, motor function, and reflexes to rule out other conditions.
- Magnetic resonance imaging (MRI): High-resolution MRI, sometimes with contrast, is used to detect vascular compression, tumors, or structural abnormalities affecting the trigeminal nerve.
- Diagnostic nerve blocks: Occasionally, a nerve block is performed to confirm the involvement of the trigeminal nerve in the pain pathway.
IGNIte Procedure: Enhancing Trigeminal Nerve Health Safely
The IGNIte procedure, offered exclusively at CSC, is a cutting-edge treatment for trigeminal neuralgia that targets nerve dysfunction safely and precisely. Performed by a board certified medical specialist, the IGNIte procedure uses advanced neurobiologics to reduce nerve hyperactivity while preserving surrounding structures.
This minimally invasive approach minimizes downtime and avoids the complications associated with traditional surgeries or radiation. Discover how this innovative technique has transformed the lives of patients suffering from trigeminal neuralgia in the video below.
Medical Management Of Trigeminal Neuralgia
Medical treatments are often the first line of defense in managing TN, with options ranging from medications to minimally invasive procedures.
- Medications: Anti-seizure medications, opioids, and lidocaine provide some relief.
- Anti-seizure medications: The following can be used for pain
- Carbamazepine: Considered the gold standard, but can cause side effects like drowsiness, dizziness, nausea, leukopenia, and a risk of Stevens-Johnson syndrome in certain populations.
- Oxcarbazepine: A similar alternative with fewer side effects.
- Others include phenytoin, valproic acid, gabapentin, pregabalin, and clonazepam.
- Opioids: Effective for acute pain but not recommended for long-term use due to dependency risks.
- IV lidocaine: Provides temporary relief in severe cases.
- Acupuncture: Acupuncture has been shown to reduce pain intensity by promoting nerve relaxation and improving blood flow, offering a non-invasive complementary option for TN management.
- Peripheral neurectomy/nerve block: These procedures involve severing or blocking the trigeminal nerve branch responsible for pain, providing relief for refractory cases.
- Surgical management: For cases unresponsive to medications, surgical options may offer long-term relief:
- Rhizotomy (nerve ablation): Burning the nerve at the foramen ovale to reduce pain signals, though it may lead to sensory complications.
- Gamma knife radiosurgery: A non-invasive option that uses focused radiation to target the nerve, with some risk of facial sensory impairment.
- Microvascular decompression: This procedure reduces pressure on the trigeminal nerve caused by nearby blood vessels. It works by gently repositioning the blood vessel and securing it away from the nerve to relieve compression.
- Balloon micro-compression: Using fluoroscopic guidance, a balloon is inflated to compress the nerve at the skull base, relieving pain by reducing nerve activity.
NSAIDs
The other day I was evaluating a patient and reviewing the treatment options for their spine condition. After discussing prior treatments, we got to the topic of medications taken for pain relief. She explained that she mainly utilized anti-inflammatory (NSAID) medications and then she told me to hold much she takes and has been for many years…..she takes close to 2 grams (2000 milligrams) on a daily basis which equated to about 9-10 capsules of medication per day. I was shocked, considering she was pre-diabetic and with high blood pressure plus the kicker of it is that her PCP (primary care physician) is ok with this…
Read More About NSAIDsPRP for Nerve Damage
Peripheral nerves are comprised of various combinations of motor, sensory, and autonomic neurons. Nerve injuries are a common condition with a broad range of symptoms depending on the severity of nerve damage which presents various challenges to patients, ranging from mild discomfort to life-long impairment. PRP for nerve damage has been shown to be effective. Let’s dig in. Nerve injuries can be classified based on the severity of damage and which structures in the nerve have been damaged. The most severe case is the complete transection of the nerve, called neurotmesis. The most common is neuropraxia from acute or chronic compression of the nerve.
Read More About PRP for Nerve DamageThere Is A Safer And More Effective Trigeminal Neuralgia Treatment
At CSC, we are committed to providing safer, non-surgical, and non-radiation alternatives for treating trigeminal neuralgia. Traditional treatments, such as invasive surgeries or radiation therapies, often carry significant risks, including nerve damage, sensory loss, or prolonged recovery times.
Our approach prioritizes innovative solutions designed to reduce pain effectively without compromising safety. When considering the potential complications of conventional options, it’s essential to explore advanced, minimally invasive techniques that deliver lasting relief with fewer risks.
Learn More About IGNIte
IGNIte is an innovative approach to nerve healing that uses regenerative biologics and image-guided precision to support nerve repair. Below, explore how this technique works and how blood platelets play a role in trigeminal nerve healing.
Have the two H3’s below in as a column section. Stack on mobile with “Understanding Interventional Neurobilogics” on top of “How Blood Platelets Repair the Trigeminal Nerve”
Understanding Interventional Neurobilogics
Interventional Neurobiologics is a cutting-edge approach designed to help injured nerves heal using precise, image-guided injections. This method targets damaged nerves, delivering regenerative biologics to promote repair and restore function. These injections utilize nerve growth factors (NGF) found in your platelets, helping to repair and restore damaged nerve fibers. This targeted approach supports recovery from conditions like trigeminal neuralgia and nerve entrapments. Watch the video below to see how Interventional Neurobiologics works and how precise injections aid nerve healing.
How Blood Platelets Repair the Trigeminal Nerve
Your body has a natural ability to heal, and blood platelets play a key role in that process. These platelets contain nerve growth factors (NGF), which help repair damaged nerves, including the trigeminal nerve. The IGNIte procedure uses advanced dual-axis fluoroscopy to pinpoint the exact area of nerve damage and deliver NGF-rich platelets where they are needed most. This precision ensures maximum effectiveness while minimizing risks. See how your own platelets can help restore nerve function—watch the video below to learn more.
Get Effective Relief For Trigeminal Neuralgia With Our Targeted Care
Trigeminal neuralgia can feel overwhelming, but effective relief is within reach at CSC. Our targeted care combines state-of-the-art treatments like the IGNIte procedure with a compassionate approach tailored to your unique needs.
Don’t let pain control your life—take the first step toward recovery with safer, more effective solutions. Schedule a consultation today and experience the difference in specialized care.
Our Doctors Who Treat Trigeminal Neuralgia

John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read moreOther Resources
-
Craniocervical Instability and Vagus Nerve Compression
Craniocervical instability (CCI) occurs when the supportive muscles and ligaments in the upper cervical spine become ‘loose’ or ‘lax’. The importance and complexity of the vagus nerve is highlighted in its name. Vagus is the Latin word for ‘wandering’ and, as the name suggests, the vagus nerve travels widely throughout the body, resembling the root…
-
Transverse Cervical Artery
The transverse cervical artery (TCA) is a branch of the thyrocervical trunk, which itself is a branch of the first part of the subclavian artery. These arteries are part of the larger arterial network that supplies blood to the head, neck, and upper limbs. Understanding the anatomy and function of arteries like the TCA is…
-
Exploring the Anatomical Structures of an Ulnar Nerve
The human body is a marvel of intricate design, and its functioning relies on a network of complex systems. Among these, the nervous system serves as the communication highway, transmitting signals that enable us to move, feel, and interact with the world around us. One crucial component of this neural network is the ulnar nerve,…
-
Guyon’s Canal Treatment Options
Growing up in South Florida, I never knew what it was like to have different seasons – we basically had hot, hotter, and blistering hot! But now being in Colorado for many years, I understand the transitions from winter to spring. It means that its time to put away my snowboard and dust off the golf…
-
PRP for UCL Injury – PRP Injections for UCL Tear
Dr. Pitts Talks About PRP for UCL Injury as an Alternative to Tommy John Surgery Transcript Hi everybody. This is Dr. John Pitts with the Centeno-Schultz Clinic, where we lead and invented much of the field of Interventional Orthopedics and regenerative medicine. Mainly we treat most musculoskeletal and orthopedic problems with injections of your own…
-
Non-Surgical Peripheral Nerve Treatment
Nerves typically become injured via compression. They get compressed in fascial layers. The compression usually happens through scar tissue formation, bone spurs, and tight muscles can compress the nerves. Tight muscles can also push the nerves into a bony prominence, or get stretched around a bone. So What Is a Hydrodissection? Non-Surgical Peripheral Nerve Treatment…
References:
Thomas KL, Vilensky JA. The anatomy of vascular compression in trigeminal neuralgia. Clin Anat. 2014 Jan;27(1):89-93. doi: 10.1002/ca.22157. Epub 2013 Feb 5. PMID: 23381734.
Docampo J, Gonzalez N, Muñoz A, Bravo F, Sarroca D, Morales C. Neurovascular study of the trigeminal nerve at 3 t MRI. Neuroradiol J. 2015 Feb;28(1):28-35. doi: 10.15274/NRJ-2014-10116. PMID: 25924169; PMCID: PMC4757119.
Hannan C, Shoakazemi A, Quigley G. Microvascular Decompression for Trigeminal Neuralgia: A regional unit’s experience. Ulster Med J. 2018 Jan;87(1):30-33. Epub 2018 Jan 31. PMID: 29588554; PMCID: PMC5849951.
Stavropoulou E, Argyra E, Zis P, Vadalouca A, Siafaka I. The Effect of Intravenous Lidocaine on Trigeminal Neuralgia: A Randomized Double Blind Placebo Controlled Trial. ISRN Pain. 2014 Mar 10;2014:853826. doi: 10.1155/2014/853826. PMID: 27335883; PMCID: PMC4893393
Xue TQ, Zhang QX, Bian H, Zhou PC, Liu C, Niu SF, Wang ZB, Shi WJ, Yan CY. Radiofrequency Thermocoagulation Through Foramen Rotundum Versus Foramen Ovale for the Treatment of V2 Trigeminal Neuralgia. Pain Physician. 2019 Nov;22(6):E609-E614. PMID: 31775414.