
Pudendal neuralgia is a condition in which the pudendal nerve becomes compressed or irritated, often due to prolonged sitting, cycling, surgical procedures, or childbirth. This nerve is responsible for providing sensation and motor functions to the pelvic area. When damaged or entrapped, it can cause chronic pelvic pain, burning sensations, numbness, increased sensitivity, and bladder and bowel dysfunction.
Pudendal neuralgia is often misdiagnosed, causing delays in receiving proper care. This can significantly impact your quality of life, affecting emotional well-being, social activities, and even everyday tasks.
At the Centeno-Schultz Clinic, we understand the importance of accurate diagnosis to identify the root causes of your pain and guide non-invasive and non-pharmaceutical treatment plans tailored to your specific needs. By addressing not just pudendal neuralgia symptoms but the underlying issues, we help you find relief and reclaim your quality of life.
What Is Pudendal Neuralgia?
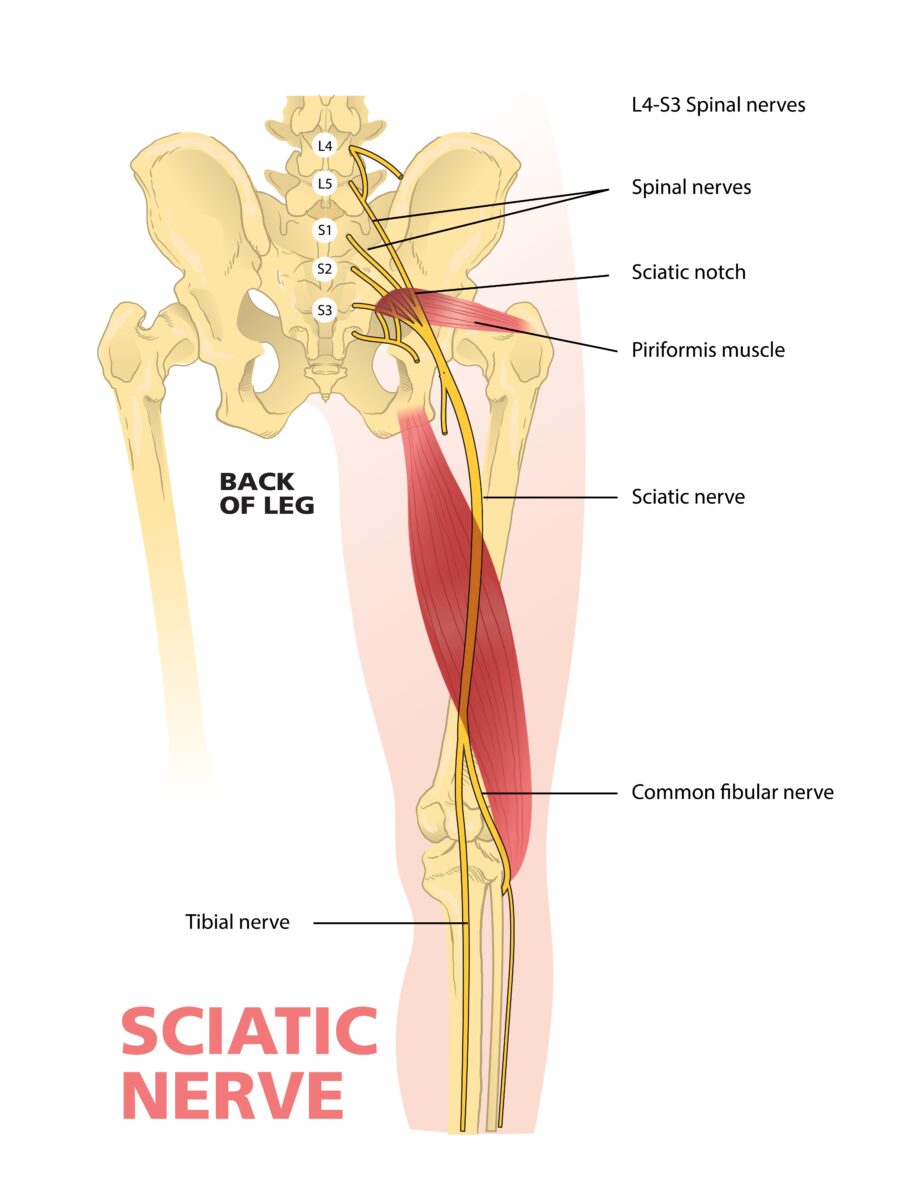
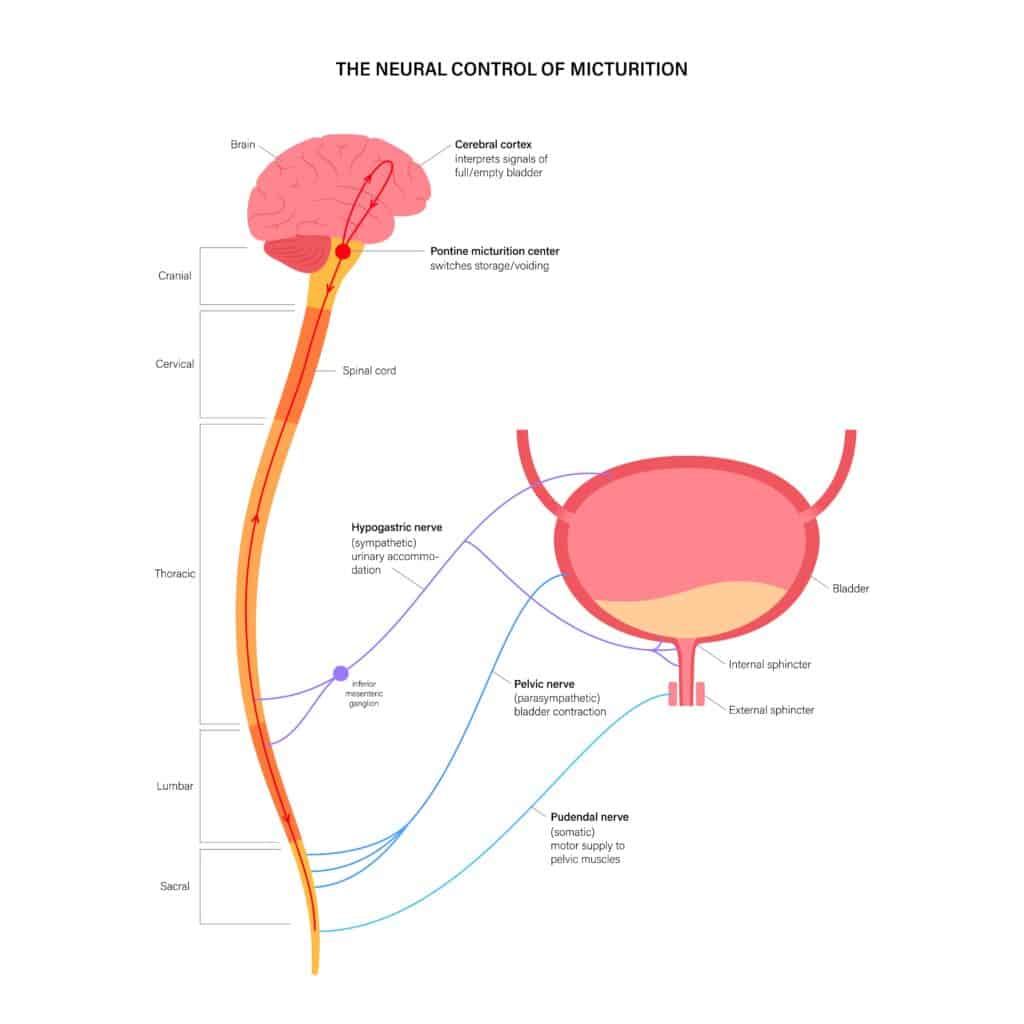
Pudendal neuralgia, also called pudendal nerve entrapment or cyclist’s syndrome, is a condition caused by compression or irritation of the pudendal nerve. This nerve originates from the spinal nerves (S2-S4) that exit the spinal column from the sacrum. From the spine, this nerve travels to the pelvic area, carrying signals from and to the brain. Its primary functions include:
- Motor: Controls muscles involved in bowel and bladder function
- Sensation: Provides feeling to your genitals and perineum

Pudendal neuralgia occurs when the nerve becomes trapped, altering nerve signaling and causing symptoms like pain, numbness, sexual dysfunction, and bladder or bowel issues. It can happen due to factors like prolonged sitting, cycling, or childbirth.
The symptoms vary significantly in type and intensity, and they often overlap with the ones of other conditions, such as sciatica. This makes it difficult to diagnose pudendal neuralgia and can delay treatment, resulting in chronic pain, reduced physical activity, and increased stress or anxiety. Research shows that, in people with misdiagnosed chronic pelvic pain, these problems can deeply affect emotional well-being and social interactions and even lead to an increased reliance on medications like opioids.
Types of Pudendal Nerve Entrapment
Pudendal nerve entrapment can happen in four main areas of the pelvis. The type of nerve entrapment is determined by the location, with each location affecting how the nerve works and causing different symptoms. Identifying the location and type of compression is important to inform treatment decisions. These types include:
Below the Piriformis Muscle
The piriformis muscle is a small, pear-shaped muscle located in the buttocks near the top of the hip joint. It plays a role in rotating and stabilizing the hip and leg. This muscle can become swollen or tight due to overuse, prolonged sitting, direct trauma, or conditions like piriformis syndrome. When this happens, it can irritate or compress tissues like the pudendal and sciatic nerves.
This type of entrapment often affects athletes or those who exercise their lower body in particular, such as cyclists.
Between Sacrospinous and Sacrotuberous Ligaments
Here, the pudendal nerve gets pinched between two ligaments in the pelvis, the sacrospinous and sacrotuberous ligaments. These are strong bands of tissue that play a role in connecting the bones of the pelvis to the lower spine (sacrum), providing stability.
If these ligaments are tight or inflamed, they can squeeze the pudendal nerve, disrupting nerve signaling between the pelvis and the brain.
Alcock Canal
The Alcock canal, also known as the pudendal canal, is a passageway located in the pelvis that allows the pudendal nerve to travel from the pelvis to the perineum.
This canal can become compressed due to inflammation or physical activity such as prolonged sitting or cycling. When the space inside the Alcock canal narrows, it can constrict the pudendal nerve, leading to pain, numbness, or tingling sensations in the pelvic region.
Entrapment of Terminal Branches
The terminal branches are the smaller endings of the nerve, responsible for reaching the genitals and perineum. They can be compressed by scar tissue or inflammation, causing pain in specific spots like the penis, clitoris, or anus.
What Are the Common Signs of this Condition?
Pudendal neuralgia can present a variety of symptoms. These are sometimes difficult to identify because they resemble those of conditions like sciatica. However, understanding common signs is important to diagnose the condition and seek appropriate care.
Common pudendal neuralgia symptoms include:
- Difficulty sitting: Activities such as sitting or cycling place additional pressure on the pudendal nerve. If this is already compressed, these activities can worsen symptoms such as pain or numbness. Pain may ease when standing.
- Burning pain in the pelvic area: Inflammation or compression of the pudendal nerve fibers results in a burning sensation in the pelvic region. This happens because the irritated nerve transmits abnormal pain signals to the brain.
- Numbness or tingling: When the nerve’s ability to transmit signals is compromised, it can lead to altered sensations like numbness or tingling in areas innervated by the nerve, such as the genitals or perineum.
- Increased sensitivity around the area: Irritated nerve fibers can process normal stimuli as painful or overly intense. This can translate into increased sensitivity in the pelvic area, causing even light touch to feel painful.
- Sexual dysfunction: The pudendal nerve plays a role in providing sensation to the genital area. When compressed or irritated, it can lead to numbness, reduced sexual function, and issues such as erectile dysfunction and difficulty achieving arousal or orgasm.
- Difficulty with urination: The pudendal nerve helps control bladder function. When compressed, it may lead to problems with urination or fully emptying the bladder. This happens because the nerve signals controlling bladder muscles are disrupted.
When Does Pelvic Discomfort Need Expert Care?
Pelvic discomfort can happen occasionally after sitting or cycling for long periods of time. However, if the discomfort does not subside after a few hours and it begins to interfere with your life, it’s time to seek expert attention.
Addressing these symptoms early on is crucial to prevent potential complications and ensure your condition doesn’t worsen. Consult with a physician if you experience:
- Persistent pain: Ongoing or severe pain in the pelvic area that doesn’t subside with rest or over-the-counter remedies and lasts for weeks.
- Pain, numbness, or tingling: These sensations in the pelvic area suggest that a nerve is compressed or irritated. Left untreated, these symptoms may worsen and interfere with daily activities and sexual function.
- Sexual and urinary issues: Difficulty urinating, controlling the bladder, or sexual dysfunction may indicate a severe issue that should not be overlooked. As these symptoms worsen, they can also impact relationships and mental health.
Avoiding Triggers That Aggravate Pelvic Pain
Managing pudendal neuralgia should involve a comprehensive approach, which includes understanding and avoiding triggers. Certain activities can increase pressure on the pudendal nerve, aggravating symptoms and delaying healing.
Here are common triggers and how to mitigate their impact:
- Prolonged or intense cycling: Cycling can compress the pudendal nerve against the bike seat, worsening discomfort and pain in the pelvic area. If you are a cyclist, consider shortening your sessions, using a well-padded, cut-out bike seat, and taking frequent breaks. Also consider adjusting the bike setup and wearing padded shorts.
- Horseback riding: Horseback riding can place pressure on the perineum and nearby structures, including the pudendal nerve. To manage symptoms, limit riding time, and use a specially-designed saddle with cushioning.
- Long-term sitting: Sitting for extended periods increases pressure on the pudendal nerve, often worsening symptoms. Possible ways to manage this aggravating factor include using cushions, ergonomic chairs, and adjustable desks. You should also stand or walk frequently: not only does this help manage symptoms, but it also supports overall health.
- Extensive workout: Intense or repetitive workouts can strain the lower body, leading to muscle tension. Tight or swollen muscles can compress the pudendal nerve and aggravate symptoms. To prevent this, find a balanced workout schedule that includes strength training, cardio, stretching, mobility, and low-impact activities like yoga. Also consider modifying exercises to reduce strain and avoiding activities that trigger pain.
How to Cope with Pudendal Neuralgia
Activity modification and lifestyle changes can help you manage the symptoms of pudendal neuralgia by easing the pressure on the pudendal nerve. Useful coping strategies include:
- Improving posture to reduce pressure: Maintaining good posture is important to allow the body to evenly distribute weight and minimize stress on the pelvic region. Practice posture exercises and invest in ergonomic chairs, desks, pillows, and mattresses.
- Avoid aggravating activities: Identify and limit activities that exacerbate your symptoms. For instance, you can try to reduce the time spent cycling or sitting, as these can increase nerve compression. Instead, focus on low-impact exercises like swimming, which are gentler on the pelvis and lower body.
- Using pillows when sitting: Utilizing cushions or seat pads can reduce direct pressure on the pudendal nerve while sitting. Ideally, opt for cushions with a coccyx cut-out or a doughnut shape to help distribute weight more evenly.
- Regular pudendal neuralgia exercises: Physical therapy and specific exercises can help by relieving muscle tension, strengthening the pelvis, and easing pressure on affected nerves. Options to try include wide leg bridges, cobra pose, child’s pose, butterfly stretch, and pelvis tilts. You may also try Kegel or pelvic floor muscles exercises to improve function.
Address the Symptoms with Centeno-Schultz’s Approach
At Centeno-Schultz Clinic, our goal is to develop comprehensive, tailored treatment plans to help you manage pudendal neuralgia and restore your quality of life. Our approach begins with a thorough diagnostic process, using advanced techniques such as ultrasound images. These allow our physician to evaluate your body in motion and determine what factors contribute to your pelvic pain.
We then use this knowledge to develop care plans that go beyond just easing symptoms and target the root cause of pain. We prioritize non-invasive, non-pharmaceutical treatments, using regenerative orthopedic approaches such as platelet lysate therapy, which promotes the body’s ability to heal naturally. This reduces reliance on medications while supporting overall pelvic health. Our aim is to help you feel better and regain your quality of life with minimal risks and less downtime compared to traditional methods like medications or surgery.
Get Reliable Solutions for Pelvic Pain Management
Pelvic pain from pudendal neuralgia doesn’t have to limit your life. At Centeno-Schultz Clinic, we offer comprehensive treatments using advanced diagnostic techniques and non-invasive regenerative orthopedics. Our goal is to empower you with a care plan that is tailored to your unique needs and targets the root cause of pain.
Struggling with pelvic pain? Schedule a consultation to address the symptoms for diagnosis and treatment options.