The PICL procedure is now 5 years old and we’re now seeing the first long-term, non-surgical craniocervical instability treatment results. This morning I’ll highlight one of those patients who I followed up on yesterday. But first, I’ll also discuss a bit of PICL history you may not know.
What is the PICL Procedure?
PICL is a craniocervical instability treatment and stands for Percutaneous Implantation of the Craniocervical Ligaments. To learn more about how the procedure works, see this video:
How Was this Craniocervical Instability Treatment Developed?
When I first began medical practice in the early 90s, fresh out of residency I met a local Ph.D. named Ed Jacobsen who performed ENG tests. These were tests to determine the cause of dizziness and imbalance.
While computerized ENG (now called VNG) tests were becoming popular with the machine telling you if the result was positive or negative and the cause, Ed did his tests the old school way, by pulling apart the data from the test and synthesizing that into a diagnosis. He was convinced that for many patients with head and neck trauma and dizziness that his tests pointed to the neck as a cause. That was highly controversial back then.
Sadly Ed passed away in 2017, but his legacy lives on.
Because of Ed, I began to see more and more patients with dizziness that had been in car crashes or had other trauma. He knew that the cause was their upper neck and I knew how to treat the neck, so I began to treat them. As time went on, most got better with simple injections to their upper neck, usually C2-C3. However, there remained a population of the most miserable patients we couldn’t help with this simple craniocervical instability treatment.
It was then that I was introduced to a local Chiropractor, Evan Katz who was using DMX. This Digital Motion X-ray technology was something I had seen before, but I didn’t quite know what to make of it. Evan convinced me that it could be useful in diagnosing patients with cervical instability, particularly upper cervical. To learn more about DMX, see my video below:
Hence, I began using prolotherapy to tighten ligaments and even published papers showing that this ligament injury happened in car crash patients and that treating it through x-ray guided injections was feasible (1,2). While some of these patients got better, in particular, the ones with craniocervical instability were harder to treat. They began to collect in my practice and were some of the patients that I was the least happy to see return because I could do nothing for them.
It was about that time that I was introduced to upper cervical fusion as a craniocervical instability treatment. The good news is that we had one or two patients who did well with this approach. The bad news was that since we were fast becoming a regional collector for patients with neck issues, headaches, and dizziness, I saw far too many that were worse after their fusions. At about this same time I was developing the Regenexx concept and using stem cells to begin to treat the damaged facet joints and ligaments of my upper cervical patients. Again, a few more got better, but there was still this group of patients that we couldn’t help.
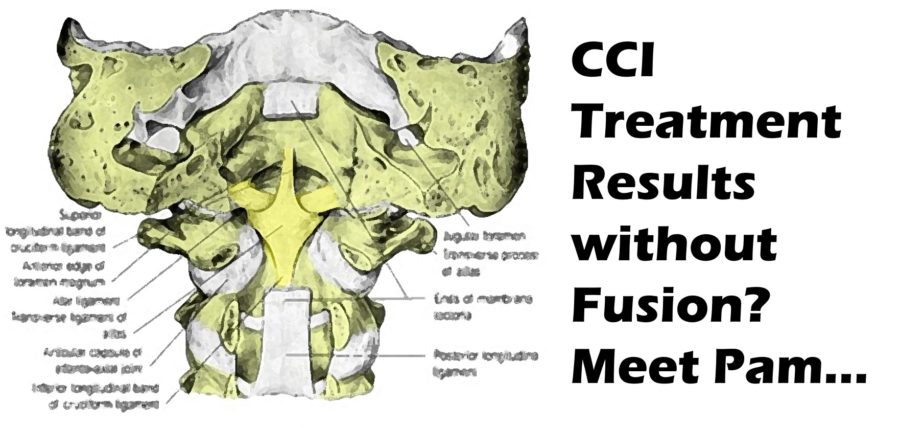
Fast forward to 2014 when I began to play with a model we had in the office looking for a better craniocervical instability treatment. This was a large C1-C2 model that had alar and transverse ligaments. I spend a year-plus looking at whether we could come in from the front to inject these ligaments.
PICL is Born
By 2015 I was convinced that you could pass a needle from the posterior oropharynx (back of the throat) through an opening in the C1-C2 bones and into the alar, accessory, and transverse ligament. While all of the anatomy textbooks said there should be nothing in the way, I was initially pretty reticent to take the plunge.
The good news was that we were seeing and publishing on dramatic results in knee ACL tears facilitated by precise x-ray guided bone marrow concentrate injections (the torn ACLs were clearly healing on post-injection MRIs) (3,4). Hence, I took the plunge and injected my first patient using an early version of the PICL procedure in 2015.
Pam’s Story
Pam was a long-time patient who was in that category that we couldn’t help. She was also good-natured about it and various injections with PRP in her spine would help this or that, but overall she remained very disabled. Then in late 2016, we decided that since she clearly had CCI, we would begin using the PICL procedure. In fact, she was one of our first patients (the 23rd procedure we did and the 12th patient we treated) .As she got these therapies, she slowly began to improve. Yesterday she was seen in the office a few months after her fourth procedure:
I have to say that I was moved by her story of dancing on New Years’ Eve. I recall that the idea of Pam dancing would have been crazy just a few years ago. While Pam was getting these procedures the PICL was advancing so that what we can reliably do today would have been very tough to replicate for her first procedure.
The upshot? It’s great to see Ed Jacobsen’s legacy live on in Pam’s life-changing craniocervical instability treatment result. If it weren’t for Ed and Evan, I don’t think the PICL treatment would be available. In addition, as a physician, you can get no greater gift than a story like Pam’s.
_______________________________________
(1) Centeno CJ, Elkins W, Freeman M, Elliott J, Sterling M, Katz E. Total cervical translation as a function of impact vector as measured by flexion-extension radiography. Pain Physician. 2007 Sep;10(5):667-71. https://www.ncbi.nlm.nih.gov/pubmed/17876363
(2) Centeno CJ, Elliott J, Elkins WL, Freeman M. Fluoroscopically guided cervical prolotherapy for instability with blinded pre and post radiographic reading. Pain Physician. 2005 Jan;8(1):67-72.
(3) Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015 Jul 31;8:437-47. doi: 10.2147/JPR.S86244.
(4) Centeno C, Markle J, Dodson E, et al. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018;16(1):246. Published 2018 Sep 3. doi: 10.1186/s12967-018-1623-3