Back pain is an epidemic and perhaps one of the most common reasons opioids and other narcotics are prescribed. You likely either know someone or are someone who has struggled with back pain for years. Depending on your pain severity and back condition, when all else fails, the F word—fusion—is likely to get thrown out for consideration. Most patients are even under the impression that a spinal fusion is the answer to getting off the narcotics they’ve been taking long term for chronic back pain. But if you’re getting a fusion to get off the opioids, you may want to think again. In fact, if you’re getting a fusion to eliminate your back pain, you may want to think again. Research suggests neither is likely. Let’s start with spinal fusion and back pain.
Don’t Count on Fusion to Relieve Your Back Pain
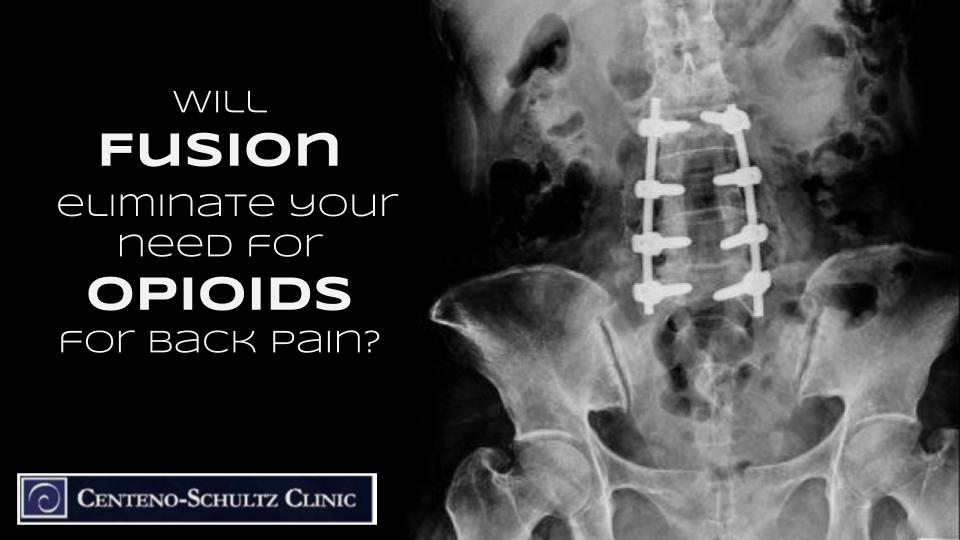
The purpose of a spinal fusion is to stop movement in a damaged area of the spine. First the disc, or discs if more than one level is involved, is removed and then the vertebrae (back bones) above and below the disc space are bolted together using screws, rods, plates, spacers, or other hardware. The vertebrae then fuse, or grow, together over time into one solid piece of bone. It sounds extreme because it is; fusion is an highly invasive surgery that often results in adjacent segment disease (ASD), which can lead to more pain, more fusions, and many other side effects. Learn more about fusion and resulting ASD by watching Dr. Centeno’s video “Should I Get a Fusion” below:
Don’t Count on a Fusion to Get Off the Opioids
After living in pain for a long time, most people who choose to have fusion surgery do so under the impression it will eliminate their back pain. They also believe they’ll be able to give up the strong side-effect-laden painkillers, such as opioids or nonsteroidal anti-inflammatory drugs (NSAIDs), which, interestingly enough may not even be helping their pain. Despite this, many fusion patients are still in pain; one study found that a huge majority (91%) never give up the opioids or other narcotics, and, in fact, nearly half (45%) actually increase their dosage.
While opioid addiction could be partially at play here, the same study found that 13% of the patients who didn’t use opioids before surgery were now using them chronically. So we wouldn’t recommend relying on fusion to get off the opioids as research has found that there is only a measly 9% chance. Even if you are one of the lucky few, you’re unlikely to dodge the ASD bullet as well.
Just Say No to an Opioid Prescription
Once you’re on opioids, it’s extremely difficult to get off opioids, so it’s best to just say no to an opioid prescription from the get-go. In addition, they may not be having the effect you’re expecting, and instead of getting pain relief, you’re only getting a possible addition that’s difficult to fight. Let’s review a few issues with opioids:
- Tylenol may be just as effective as opioids at pain relief.
- After a knee replacement, you’re likely to experience more pain following surgery if you were on opioids prior to surgery.
- Opioid can actually have a reverse effect on pain, disrupting pain signals and amplifying chronic pain.
- Think one 10-day opioid prescription is no big deal? Think again—there’s a 20% chance of addiction to this dangerous narcotic with just one prescription .
We have seen spinal fusions create more horror stories in patients lives than any other surgical procedure. Using fusion to get off the opioids by eliminating your pain, is something the bulk of the literature simply doesn’t support this. Make sure you meet with your interventional orthopedic physician to review your nonsurgical alternatives to fusion, because going into a surgery with the hopes of being one of the rare and lucky few is simply never a good idea!