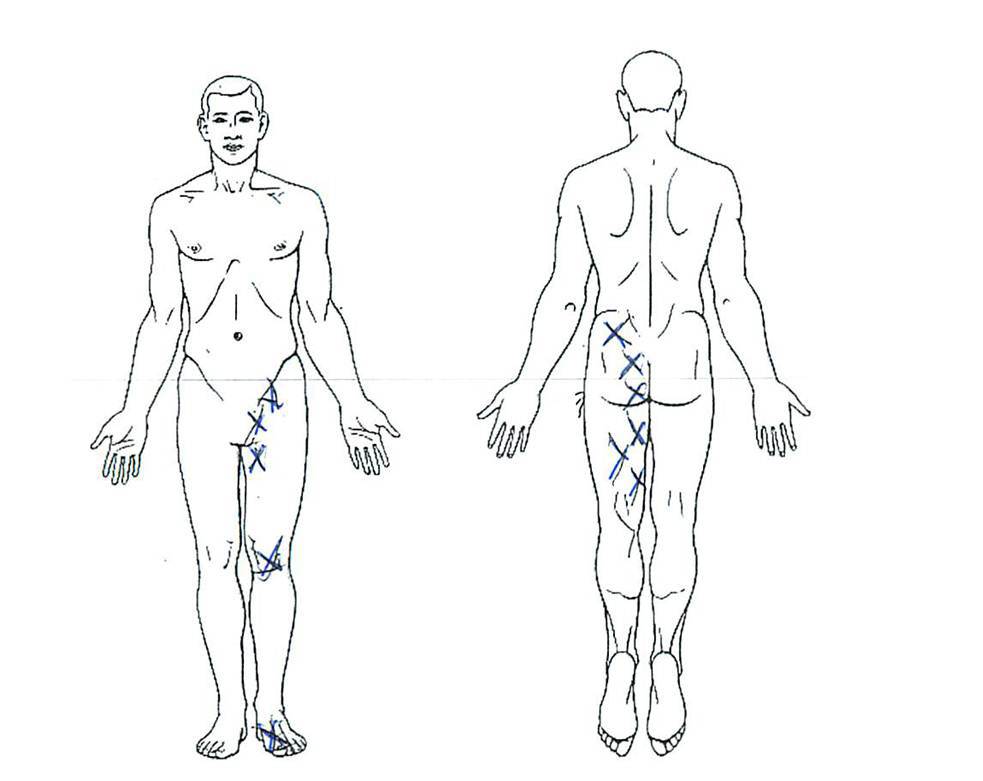
Our first experience with misdiagnosed patients and big hip surgery was many years ago. A patient came into the office with severe hip pain and was unable to get in or out of her car. An x-ray showed hip arthritis, so she was told she needed a surgery to install a new hip. Wanting to avoid hip surgery, she came to us and we found extensive muscle trigger points throughout her hip and low back. Four trigger point IMS treatments later, her hip pain was gone and she avoided the hip surgery. A second example was a doctor’s wife who had hip pain and was told her MRI showed a congenital hip problem, so at barely 40, she was a hip surgery candidate. On exam she had clear evidence of a pinched nerve in her low back, so instead we focused on the Regenexx-PL disc procedure, which took away her hip pain. The concept of a false positive hip diagnosis leading to unnecessary surgery has been published by others as well. That takes us to the pain diagram above of a patient who was told she needed hip labrum surgery. The hip labrum is the lip of the socket where the ball of the hip inserts. It’s function is to help hold the ball in the socket. Finding and treating labral tears has exploded in recent years, with MRI’s of the hip now coming back with a read on the labrum showing tears that seemed to be non-existent just a few years ago. Surgery to treat a hip labrum tear is intense and may involve serious complications. One concern we have is that 80-100 pounds of traction can be pulled on the hip to pull the ball of the hip joint out of the socket, which opens up working room for the arthroscope. The hip labrum tear can be sewn back together or sometimes the bone spur (often found at this spot in the hip) is removed and the entire outer portion of the hip is restructured. As a physician, while the procedure may be needed in select patients, my concerns are that our own experimental cadaver studies have shown that pulling less traction on the hip injured the important ligament that holds the hip in the socket and that the surgery cuts off nerve supply (femoral nerve) to the leg for 1-2 hours (the nerve is monitored carefully). Amid all of that history, walks this patient this morning with the pain diagram above. She’s in her thirties and very active and suddenly a few months ago began to have groin pain that prevented her from hiking. A few weeks later she began to have pain and tightness down that leg (as shown above). The problem with the pain diagram is that it looks nothing like someone with primary hip pain (which is usually groin, sometimes outside of hip pain). Instead, this looks allot more like someone who has a pinched nerve in their low back. While her MRI showed a small labral tear, a hip steroid and anesthetic injection didn’t take her pain away. As a result, I had to wonder why invasive hip labrum surgery is being recommended. Are there other ways to treat a hip labrum tear? If it’s actually causing symptoms (as one example a recent study that showed that most meniscus tears in middle aged people likely aren’t causing pain), then why not try injecting the patient’s own platelets and stem cells into the torn hip labrum before surgery? the Regenexx-SCP or Regenexx-SD procedures would be our first choice with injections under x-ray or MSK ultrasound guidance into the hip labrum tear to promote healing. Rather than put this patient through an invasive hip surgery or even consider a stem cell injection, today I recommended a trial of IMS trigger point deactivation as well as a low back MRI!