Radial Nerve Palsy
Radial Nerve Palsy is a term we use when there has been an injury to the radial nerve. Commonly the nerve becomes compressed and affects the function of the nerve leading to weakness in the muscles innervated by the nerve, such as in a wrist drop. Today we are going to take a deep dive into the details of radial nerve injuries and what can be done to help.
What Is the Radial Nerve?
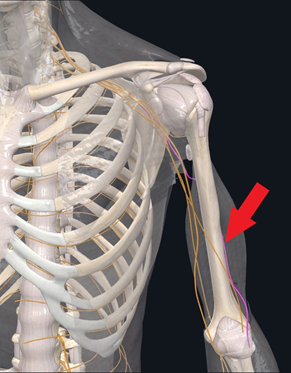
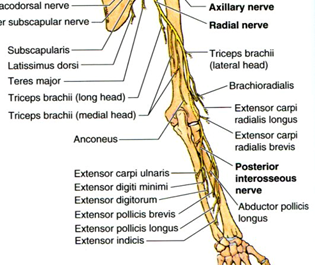
The radial nerve is the largest nerve in the upper limb. It starts in the shoulder and travels through the forearm to the back of the wrist. It has nerve fibers from C5, C6, C7, C8, and T1 nerve roots. Radial nerve palsy = damage to the radial nerve which affects the muscles the nerve goes to, creating weakness in those muscles, clinically presenting with wrist drop….the inability to extend the wrist. But the radial nerve innervates many muscles of the upper arm and forearm. See the list below:
Innervated Muscles of the Radial Nerve:
- Abductor Pollicis Longus — abduct the thumb at the wrist.
- Extensor Carpi Ulnaris — extends and adducts the wrist.
- Extensor Dminimi — extends the wrist and small finger.
- Extensor Digitorum — extends the medial four digits of the hand.
- Extensor Indicis — extends the index finger and to some extent wrist extension.
- Extensor Pollicis Brevis — extends and abducts the thumb at the carpometacarpal and metacarpophalangeal joints.
- Extensor Pollicis Longus — extends the terminal phalanx of the thumb.
Posterior interosseous nerve (PIN):
- Abductor Pollicis Longus — abduct the thumb at the wrist.
- Extensor Carpi Ulnaris — extends and adducts the wrist.
- Extensor Digiti Minimi — extends the wrist and small finger.
- Extensor Digitorum — extends the medial four digits of the hand.
- Extensor Indicis — extends the index finger and to some extent wrist extension.
- Extensor Pollicis Brevis — extends and abducts the thumb at the carpometacarpal and metacarpophalangeal joints.
- Extensor Pollicis Longus — extends the terminal phalanx of the thumb.
Symptoms of radial nerve palsy depend on where along the course of the nerve the compression or damage occurs! Any muscles innervated distally (towards the fingers) to the lesion will be affected.
How Long Does Radial Palsy Last?
When injured, nerve recovery varies widely taking weeks, months, and in some cases years to recover. Addressing the underlying cause is critical. Factures, soft tissue swelling, or tight muscles can all lead to nerve compression causing radial nerve palsy. Nerve recovery typically occurs at a rate of 1-3mm per day! In some cases, the damage can be permanent if not treated in a timely fashion!
What Causes Radial Nerve Palsy?
Along the course of the radial nerve, several common areas that the nerve innervates can become damaged, leading to radial nerve palsy. Those conditions are discussed below:
Radial Nerve Palsy

Radial neuropathies occur from injury to the radial nerve due to compression, ischemia, fractures to the arm, or penetrating wounds. Wrist drop is the most common presentation. The severity of the neuropathy depends on the level of the injury. Palsy of the radial nerve is also known as crutch palsy, Saturday night palsy, and honeymooner’s palsy, conditions which may occur after placing one’s arm over a chair (or crutches) for an extended period causing a pressure injury to the radial nerve.
Radial Tunnel Syndrome
Radial Tunnel Syndrome presents with symptoms including fatigue or dull, aching pain in the forearm during use. Less commonly these symptoms can occur at the back aspect of the wrist or hand. Radial Tunnel Syndrome typically occurs secondary to overuse or repetitive movements from pushing, pulling, gripping, pinching, or bending at the wrist typically from a job or playing sports. Muscle overuse may cause compression of the radial nerve anywhere along its path, but most commonly occurs over the elbow as it passes through the radial tunnel. Commonly misdiagnosed as “Tennis Elbow” but eventually diagnosed when all treatments of tennis elbow do not help!
Radial Nerve Entrapment
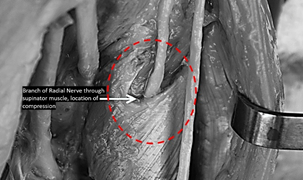
Radial nerve injury or compression can occur anywhere along the nerve’s path which can cause extensor or supinator muscle denervation. This can result in pain, weakness, dysfunction, or paresthesias and numbness along with the sensory distribution of the radial nerve. The proximal forearm is the most common area of compression where the posterior interosseous branch of the radial nerve passes between the supinator heads. Other, less common, sites of compression can occur due to fractures of the humerus about the middle and proximal thirds of the shaft. The radial aspect of the wrist is another site of possible compression of the radial nerve. Treatment for radial nerve entrapment depends on the pathology and may be treated conservatively or surgically if conservative measures fail.
Cheiralgia Paresthetica (Wartenberg syndrome)
Cheiralgia paresthetica is a hand neuropathy commonly caused by trauma or compression of the superficial branch of the radial nerve. The dorsum of the hand near the base of the thumb (in the vicinity of the anatomical snuffbox) is typically affected; however, it may affect the dorsum of the thumb, index finger, and hand. Symptoms include pain, numbness, tingling, or a burning sensation. There is no motor involvement since the superficial branch is purely sensory. Its etiology is thought to be caused by a constriction of the wrist as with a watch band or bracelet. It is associated with handcuff use and is also commonly referred to as handcuff neuropathy.
Symptoms Associated With Radial Nerve Injuries
Arm Pain at Night
Arm pain at night can be miserable. The pain can interrupt your sleep and erode your quality of life. Irritability becomes increasingly more common. What are the causes? When should I worry about it? What are the treatment options for arm pain at night? The neck is composed of 7 boney building blocks numbered 1- 7. Sandwiched between the bones is a disc that functions as an important shock absorber. The cervical discs are susceptible to injury due to trauma, degeneration, repetitive motion, and surgery. Common disc injuries include disc bulges, and herniations. The injured disc can compress or irritate one or more nerves resulting in arm pain at night. It can…
Read More About Arm Pain at NightArm Throbbing
In many patients, irritated neck nerves don’t present as a symptom in the neck. In fact, sometimes the only symptoms of irritated nerves in the neck occur in the arm muscles, as either tightness, throbbing, or both. While the arm throbbing might be frustrating as it’s happening, you might not think a whole lot about it, especially if it only happens on occasion. However, ignoring it is not a good idea since it is often a warning signal of a bigger problem in the neck. These body connections occur all the way back to when we were a fetus, like the neck, shoulder, and arm.
Read More About Arm ThrobbingFeeling Of Pins And Needles In Fingers
Are you experiencing the sensation of pins and needles in your fingertips? This is a common symptom of cervical radiculopathy. Although many conditions can cause pins and needles, if it is accompanied by neck pain, then cervical radiculopathy would be at the top of the diagnostic list. Cervical radiculopathy also referred to as a “pinched nerve.” is a medical syndrome that occurs when a nerve root in the neck ( cervical spine) becomes compressed or irritated leading to symptoms that include pain, numbness, tingling, and potentially weakness. It occurs in about 85 people per 100,000 (1). Read this post to find out more about cervical radiculopathy and how it can cause pins and needles in your fingertips.
Read More About Feeling Of Pins And Needles In FingersHands Stiff in the Morning
Hand stiffness can make simple tasks overwhelming. Why are my hands stiff in the morning? What are the treatment options for hand stiff in the morning? Are there new, natural treatment options to treat hands that are stiff in the morning? Our hands are central to virtually everything we do. Stiffness can compromise function and cause pain. What are the causes of hand stiffness in the morning? There are many which include: excessive daily wear and tear, medications that can cause hand swelling and stiffness. Common examples include hormones, calcium channel blockers for high blood pressure, steroids, anti-depressants, and NSAIDs, Diets high in salt, alcohol, and trauma.
Read More About Hands Stiff in the MorningLeft Arm Numbness
Treatment depends upon the underlying cause of the arm numbness. Left-arm numbness is a warning sign that requires attention. As noted above unexplained numbness requires immediate attention. At the Centeno-Schultz Clinic, we are experts in the treatment of left-arm numbness due to cervical nerve irritation, cervical stenosis, thoracic outlet syndrome, and peripheral nerve injuries. When appropriate first-line treatment should involve conservative care including physical therapy and stretching. Steroid injections should be avoided as they are toxic to orthopedic tissue and can accelerate damage. Surgery for Cervical Stenosis and Thoracic…
Read More About Left Arm NumbnessMotor Issues
Cervical radiculopathy is a condition caused by compression of a cervical nerve root, which can result in pain and sensorimotor deficits. Nerve roots are mixed nerves which are responsible for sensory and motor function. There are eight cervical nerve roots that branch off from the spinal cord, labeled from C1-C8. Each cervical nerve root supplies a particular region of skin, called a dermatome,and innervates certain groups of muscles, called a myotome. When the cervical nerve root is compressed, the sensory supply to the dermatome in the upper limb can be altered. This can lead to pain, decreased sensation, the feeling of pins and needles, and even numbness. This can also coincide with muscle weakness, and a decreased reflex response.
Read More About Motor IssuesTingling Sensation in the Hands
Have you ever felt the sensation of a thousand tiny pins and needles pricking your hands or the subtle, electric tingling that runs down your fingers like a gentle current? Tingling sensations in the hands are more common than you might think and can be triggered by a multitude of factors, from temporary nerve compression to chronic medical conditions. While often dismissed as a momentary inconvenience, this seemingly innocuous tingling can sometimes be a signal from your body, a signpost pointing to underlying health concerns. In this article, we delve into the intriguing world of tingling sensations in the hands, unraveling the causes, potential implications, and, most importantly, what you can do to address them.
Read More About Tingling Sensation in the HandsDiagnosing Radial Nerve Palsy
Ultrasound
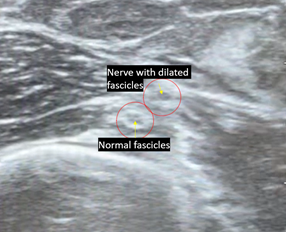
Ultrasonography can precisely visualize the anatomical integrity of the nerve, differentiating between a rupture of the nerve, localized swelling around the nerve, and neuroma formation. It can demonstrate the exact location of the nerve injury and follow the nerve along its anatomical path. It is non-invasive, affordable, and has specific advantages over MRI and other diagnostic procedures.
Physical Examination
Physical Examination of all the muscles innervated by the radial nerve can be tested for strength and function, including the triceps, forearm supinator, and wrist and finger extensors. For the upper lesions of radial nerve, loss of elbow extension should be evaluated with gravity eliminated. The examiner should be aware that with digital flexion, some extension of the wrist is possible with tight passive extensors. Digital extension is an area where most errors in diagnosis can occur. Extension of interphalangeal (IP) joints is accomplished by the interossei and lumbrical muscles innervated by the ulnar nerve. With radial nerve injury, only extension in the MCP joints is affected. One can also test the sensation on the dorsum of the hand and lateral three and a half fingers as well as the arm and forearm.
EMG / NCS

Electromyography and nerve conduction (EMG/NCS) electrodiagnostic studies are helpful when trying to locate anatomically a nerve lesion. One can differentiate between cervical radiculopathies, brachial plexopathies and peripheral nerve lesions. One can also monitor nerve recovery during the period of rehabilitation, especially from four months, when regeneration can be detected.
How Do You Treat Radial Nerve Palsy?
Rest, activity modification, non-steroidal anti-inflammatory drugs (NSAIDs), vitamin therapy, and a period of immobilization in a functional splint are the typical initial treatment strategies.
- Brace

- PT
- EMG to follow recovery
- Brachioradialis first to recover
- One of the most important aspects of this treatment is to maintain a full passive range of motion in all the affected joints through exercise programs and the use of dynamic splints. The key function attributable to the radial innervated muscle is wrist extension.
- EMG to follow recovery
- Surgical Nerve Exploration (with or without nerve repair)
- the nerve can be repaired by direct suturing or nerve grafting. Other reconstructive procedures such as tendon transfers may also become necessary to overcome any permanent nerve dysfunction. Nerve transfers and functional free muscle transfers are currently gaining in popularity.
- Recovery of radial nerve motor function may be expected if the repair is carried out within 15 months of the injury
- Radial nerve function can be restored through the direct nerve transfer of the motor branches of the median nerve in the proximal forearm to the extensor carpi radialis brevis and the posterior interosseous branches of the radial nerve. The branch to the pronator teres muscle can be transferred to the extensor carpi radialis longus branch. The branch to the flexor carpi radialis is used to revive the posterior interosseous nerve. The flexor digitorum superficialis tendon can also be transferred to the extensor carpi radialis brevis tendon to recreate wrist extension. The success of these procedures is gauged by testing the degree of resultant wrist and finger extension
The Newest Technique
We have been successfully using a Percutaneous Nerve Hydro-Dissection Release for many years with excellent results. We use the patient’s own platelet-derived growth factors that can promote nerve healing through cytokines like NGF, PDGF, and IG-1.
The use of the patient’s own platelets has been shown to be superior to steroid shots in the treatment of carpal tunnel syndrome. PRP has also been shown to be superior to using another commonly injected substance called D5W. Others have also found good results with this platelet based injection technique.
Example of this technique:
To see how we can help in your case, please use the phone number or Appointment button here: centenoschultz.com
References:
Sowa Y, Kishida T, Tomita K, Adachi T, Numajiri T, Mazda O. Involvement of PDGF-BB and IGF-1 in activation of human Schwann cells by platelet-rich plasma. Plast Reconstr Surg. 2019 Aug 27. doi: 10.1097/PRS.0000000000006266. Schwann Cell-Like Cells: Origin and Usability for Repair and Regeneration of the Peripheral and Central Nervous System (nih.gov)
Shen YP, Li TY, Chou YC, Ho TY, Ke MJ, Chen LC, Wu YT1. Comparison of perineural platelet-rich plasma and dextrose injections for moderate carpal tunnel syndrome: A prospective randomized, single-blind, head-to-head comparative trial. J Tissue Eng Regen Med. 2019 Jul 31. doi: 10.1002/term.2950. Comparison of perineural platelet-rich plasma and dextrose injections for moderate carpal tunnel syndrome: A prospective randomized, single-blind, head-to-head comparative trial – PubMed (nih.gov)
Karabay N, Toros T, Ademoğlu Y, Ada S. Ultrasonographic evaluation of the iatrogenic peripheral nerve injuries in upper extremity. Eur J Radiol. 2010 Feb;73(2):234-40. doi: 10.1016/j.ejrad.2008.10.038. Epub 2008 Dec 11. PMID: 19084364. https://pubmed.ncbi.nlm.nih.gov/19084364/
Peer S, Bodner G, Meirer R, Willeit J, Piza-Katzer H. Examination of postoperative peripheral nerve lesions with high-resolution sonography. AJR Am J Roentgenol. 2001 Aug;177(2):415-9. doi: 10.2214/ajr.177.2.1770415. PMID: 11461873. https://pubmed.ncbi.nlm.nih.gov/11461873/
Lee FC, Singh H, Nazarian LN, Ratliff JK. High-resolution ultrasonography in the diagnosis and intraoperative management of peripheral nerve lesions. J Neurosurg. 2011 Jan;114(1):206-11. doi: 10.3171/2010.2.JNS091324. Epub 2010 Mar 12. PMID: 20225925. https://pubmed.ncbi.nlm.nih.gov/20225925/
Hassan DM, Johnston GH. Safety of the limited open technique of bone-transfixing threaded-pin placement for external fixation of distal radial fractures: a cadaver study. Can J Surg. 1999 Oct;42(5):363-5. PMID: 10526521; PMCID: PMC3788902. https://pubmed.ncbi.nlm.nih.gov/10526521/
Lim R, Tay SC, Yam A. Radial nerve injury during double plating of a displaced intercondylar fracture. J Hand Surg Am. 2012 Apr;37(4):669-72. doi: 10.1016/j.jhsa.2012.01.002. Epub 2012 Feb 25. PMID: 22365823. https://pubmed.ncbi.nlm.nih.gov/22365823/
Lin CC, Jawan B, de Villa MV, Chen FC, Liu PP. Blood pressure cuff compression injury of the radial nerve. J Clin Anesth. 2001 Jun;13(4):306-8. doi: 10.1016/s0952-8180(01)00262-8. PMID: 11435057. https://pubmed.ncbi.nlm.nih.gov/11435057/
Noger M, Berli MC, Fasel JH, Hoffmeyer PJ. The risk of injury to neurovascular structures from distal locking screws of the Unreamed Humeral Nail (UHN): a cadaveric study. Injury. 2007 Aug;38(8):954-7. doi: 10.1016/j.injury.2007.04.014. Epub 2007 Jul 12. PMID: 17631884. https://pubmed.ncbi.nlm.nih.gov/17631884/
Blyth MJ, Macleod CM, Asante DK, Kinninmonth AW. Iatrogenic nerve injury with the Russell-Taylor humeral nail. Injury. 2003 Mar;34(3):227-8. doi: 10.1016/s0020-1383(01)00176-0. PMID: 12623256. https://pubmed.ncbi.nlm.nih.gov/12623256/ Glover NM, Murphy PB. Anatomy, Shoulder and Upper Limb, Radial Nerve. [Updated 2020 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available https://www.ncbi.nlm.nih.gov/books/NBK534840/