Doctors often describe pain after spinal fusion as “normal,” but this expectation warrants scrutiny. Such pain can signal complications, inadequate pain management, or issues with the surgical procedure itself. Normalizing pain may lead to patients ignoring serious symptoms, delaying necessary interventions and causing permanent injuries.
Understanding why pain persists and addressing it effectively is crucial for proper recovery and overall patient health. This article delves into the reasons behind post-surgical pain and the importance of reevaluating its acceptance as a standard outcome.
Where Does Pain After Spinal Fusion Happen?
After spinal fusion, here are parts of the body that can experience pain:
- Lower back: The fusion site often experiences pain due to removal of discs, bone, ligaments, tendons, muscle along with insertion of cages, bone grafts, screws, bolts and rods.
- Down the leg: Known as radiculopathy or sciatica, this pain can occur if nerve irritation, inflammation, or injury occurs from the surgery.
- Around the incision site: Pain can be present around the surgical incision due to the healing of skin, muscle, and other tissues.
- Neck: If the fusion is in the cervical spine, pain may radiate to the neck and shoulder areas.
- Adjacent vertebrae: The vertebrae above and below the fusion site can experience pain due to increased stress and motion.
Types Of Pain After Spinal Fusion
Types of pain after spinal fusion can include:
- Numbness: A tingling or loss of sensation, often resulting from nerve irritation or compression or injury during the surgery.
- Weakness: A reduction in muscle strength, potentially due to nerve or muscle damage following surgery.
- Loss of function: Difficulty performing daily activities or movements, which may arise from pain, stiffness, weakness, or nerve-related issues impacting mobility and coordination.
Causes Of Pain After Spinal Fusion
Possible causes of pain after spinal fusion can include:
- Failed fusion: Incomplete or unsuccessful fusion of the vertebrae, leading to instability and persistent pain. This is a medical condition where the bones fail to fuse.
- Hardware problems: Issues with surgical implants, such as screws or rods, which can become loose, fractured, or actually break, thereby causing instability and pain.
- Poor posture: Incorrect posture post-surgery can place undue stress on the spine and surrounding muscles, leading to pain.
- Nerve injury: Compression or irritation of spinal nerves during or after the surgery, causing pain, numbness, or weakness.
- Inadequate diagnosis pre-surgery: Failure to accurately identify all sources of pain before surgery, resulting in unresolved or new pain issues post-operation.
Complications From Spinal Fusion
Here are some complications from spinal fusion:
ASD
Adjacent segment disease (ASD) simply means that the area above and below the fusion is getting overloaded (3). This happens when one part of the spine is fused and the energy and movement that used to be handled by that segment has to get directed elsewhere.
Hence, it tends to go above and below the fusion, leading to an overload of the discs and facets above and below the fusion, leading to additional wear and tear. For more information, see my video below:
Dead Muscles
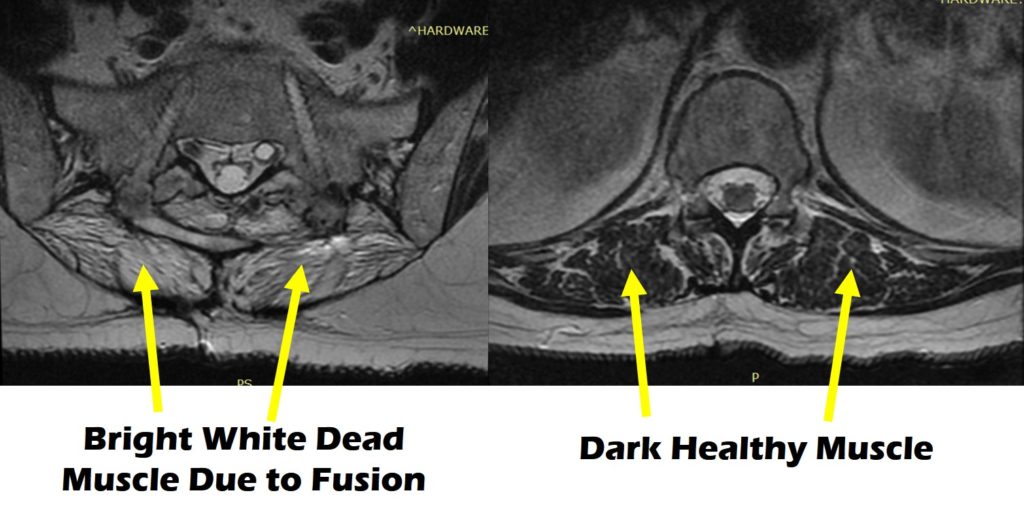
Muscles in the spine are key stabilizers of the spine and allow for motion. Unfortunately, surgery can compromise the integrity of the spine muscles. In many cases, after spinal fusion, the muscles can become weakened or severely atrophied.
A recent study looked at the effects of single-level fusions on spine muscle health (1). What did they find? That the low back muscles had atrophied (got smaller) and had shrunk about 50% due to the surgery! What are the implications of this?
These muscles are used to help bend over, pick up things, and carry stuff. When they atrophy, it becomes tough to do these things. Hence, the loss of these muscles is not a good thing as it compromises movement and stability.
Infection
Infections are a serious complication. They may occur in the skin, muscle or bone requiring antibiotic therapy. In severe cases, all the surgical hardware such as screws, bolts, plates, and cages must be removed until the infection is successfully treated.
Post-surgical infections at the incision site or deeper within the surgical area, can cause pain and swelling and require additional treatment.
Blood Clots
Deep vein thrombosis (DVT) can occur after surgery, leading to potentially serious complications if the clots travel to the lungs or other parts of the body.
Nerve Damage
Damage to nerves and/or the spinal cord during surgery can result in chronic pain, numbness, weakness, or loss of function.
Hardware Complications
Problems with the surgical implants, such as loosening, breaking, or irritating surrounding tissues, may require additional surgeries.
Nonunion
The bones may fail to fuse properly, a condition known as nonunion or pseudarthrosis, leading to ongoing pain and instability. In many cases, additional surgery is required.
Persistent Pain
Some patients may continue to experience chronic pain despite successful fusion, potentially due to nerve issues, scar tissue, instability, or inaccurate preoperative diagnosis.
Limited Mobility
Reduced range of motion and flexibility in the fused segment of the spine, which can impact daily activities and quality of life.
Remedying The Pain After Spinal Fusion
The pros and cons of prescribing more surgery:
Pros:
- Address underlying issues: Additional surgery may potentially address surgical complications or unresolved issues such as hardware problems, failed fusion, or nerve compression, potentially providing long-term relief.
- Improved stability: Corrective surgery can enhance spinal stability if the initial fusion did not achieve the desired outcome. This requires additional surgeries which have risks and complications. In general, less surgery is better.
Cons:
- Increased risk of complications: Additional surgeries carry inherent risks, such as infection, blood clots, and further nerve damage, which can exacerbate pain and lead to additional health issues. Surgery forever changes the biomechanics of the spine.
- Extended recovery time: Another surgery often requires a prolonged recovery period, causing more downtime and impacting the patient’s ability to resume normal activities.
- Cost and financial burden: The financial costs of additional surgeries can be significant, including hospital fees, surgeon fees, and the cost of follow-up care and rehabilitation. Given these rising expenses, patients are increasingly turning to digital financial solutions, such as researching the best crypto wallet UK, to manage healthcare-related transactions efficiently. This trend highlights the broader need for accessible financial tools to ease the burden of medical expenses.
- Uncertain outcomes: There is no guarantee that additional surgery will resolve the pain, and in some cases, it may lead to persistent or worsened symptoms, leading to further frustration and distress for the patient.
- Limited Mobility: As discs are moved and hardware inserted, patient mobility decreases.
- Persistent Pain: Pain post-fusion is real. It may be similar or worse than the pain prior to the procedure. OpioIds have significant side effects including addiction.
Do New Treatment Options Exist For Pain After Spinal Fusion?
The short answer is yes; alternatives to spinal fusion do exist. For example, we treat ASD quite frequently by using newer interventional orthopedic techniques above and below the fusion.
Here’s how:
- Natural substances derived from the patient’s body: We use growth factors derived from platelets to prompt or stimulate healing in these affected areas.
- Precise injections: These injections are placed precisely with fluoroscopy or ultrasound to ensure targeted treatment.
- Avoiding harmful traditional approaches: Traditional approaches like steroids and radiofrequency can harm and break down spine tissue, which we avoid.
The upshot? Pain that occurs months to years after fusion surgery is real. It can be mild to severe, compromising function and wellbeing. Post-fusion pain can arise from many different sources, and for that reason, it is important to secure an accurate diagnosis.
At the Centeno-Schultz Clinic, we are committed to providing each patient with an accurate diagnosis. It starts with a complete history that includes review of current complaint, onset of pain, aggravation, alleviating factors, and treatment to date. Past medical, surgical history, and current medications are reviewed.
A physical examination is performed that includes an evaluation of motor strength, sensation, and range of motion. Current imaging including x-rays, MRI’s and CAT scans are reviewed.
The information outlined above is then used to establish an accurate diagnosis.
The most common causes of post-fusion pain include:
- Degeneration or injury of the disc above or below the fusion
- Degeneration or injury of the facet joints at, below, or above the level of the fusion
- Spinal instability due to ligament laxity or muscle weakness
- Spinal stenosis
- Nerve irritation
- Sacroiliac joint dysfunction or instability
Treatment does NOT include surgery. Rather, it includes regenerative therapies for the areas of injury and instability.
Diagnostic procedures: Comprehensive diagnostic procedures are used to accurately identify the root cause of pain.
- Advanced imaging techniques: Use of MRI, CT scans, and X-rays to get a detailed view of the spine and surrounding tissues.
- Fluoroscopic guidance: Use of real-time X-ray technology to precisely identify problem areas during diagnostic and treatment procedures.
- Electrodiagnostic testing: Performance of nerve conduction studies and electromyography (EMG) to assess nerve function and detect any abnormalities.
- Functional assessments: Conducting physical exams and functional tests to understand the impact of pain on movement and daily activities.
Non-surgical procedures: Minimally invasive treatments designed to promote natural healing and repair. They include:
- Platelet-rich plasma (PRP) treatment: Uses concentrated platelets from the patient’s blood to stimulate tissue repair and reduce inflammation.
- Prolotherapy: Injects natural irritants to stimulate the body’s healing response in ligaments and tendons around the spine.
- Regenerative injection treatment: Uses injections that contain growth factors and cytokines to repair and regenerate spinal tissues.
- Physical therapy and rehabilitation: Implements tailored physical therapy programs to strengthen muscles, improve flexibility, and enhance recovery.
Pain After Spinal Fusion Shouldn’t Be Perceived As Normal
At CSC, we believe that pain after spinal fusion should not be accepted as a normal part of recovery. Our philosophy is centered on identifying and addressing the root causes of pain through comprehensive diagnostic procedures and innovative, non-surgical treatments.
By utilizing advanced imaging techniques, precise injections, and regenerative therapies, we aim to promote natural healing and tissue repair without the need for additional surgeries.
Our approach prioritizes patient well-being and long-term recovery, offering effective alternatives that enhance quality of life and restore functionality. At CSC, we are committed to treating spinal conditions and back pain with cutting-edge, patient-focused care.
Break free from the cycle of pain. Make an appointment with us today!