Understanding Why You Are Experiencing Abnormal Reflexes
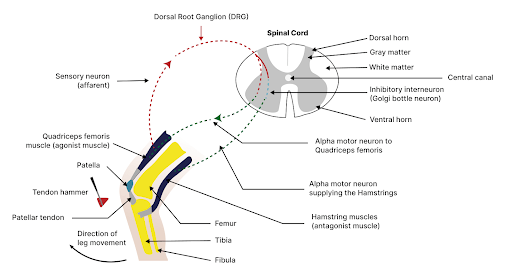
Get Help With Abnormal ReflexesDeep tendon reflexes (DTRs) are involuntary responses of muscles to a sudden stretch, typically elicited by a sharp tap from a reflex hammer on a tendon. They work through a simple neural circuit known as the monosynaptic reflex arc.
When a tendon is tapped, the muscle attached to it is quickly stretched, stimulating specialized sensory receptors called muscle spindle fibers. These receptors then send an impulse via afferent (sensory) neurons to the spinal cord, where they directly synapse with efferent (motor) neurons.
These motor neurons immediately convey an impulse back to the same muscle, causing it to contract reflexively. This reflex arc bypasses conscious control in the brain, enabling a rapid response. DTRs are important clinical tools, as they help assess the integrity of the peripheral and central nervous systems. Changes in reflexes can indicate neurological disorders or damage to specific neural pathways.
The Mechanism of Reflex Actions
Reflexes are fundamental physiological responses in the body, involving several key anatomical structures:
- Receptors (sensory organs): Reflexes begin at sensory receptors, which are specialized structures located in muscles, tendons, and joints. In the context of DTRs, muscle spindle fibers play a crucial role. These are sensitive to changes in muscle length, detecting stretch when a tendon is tapped.
- Sensory (afferent) neurons: When a receptor such as a spindle is stimulated, it generates an electrical impulse. This impulse is carried by sensory neurons, which transmit information from the receptor to the spinal cord. These neurons have a sensory nerve ending at the receptor and a terminal end in the spinal cord.
- Spinal cord and synapse: The spinal cord serves as the central pathway for transmitting neural signals. Here, the sensory neurons form synapses with motor neurons. In simple reflex arcs, like the knee-jerk reflex, this synapse is monosynaptic, meaning there is a direct connection between the sensory and motor neurons without any interneurons.
- Motor (efferent) neurons: These neurons carry the impulse from the spinal cord to the effector muscles. They are responsible for executing the response to the stimulus.
- Effector muscles: Upon receiving the signal via motor neurons, these muscles react accordingly. In reflex actions, this usually results in muscle contraction. For example, when the patellar tendon is tapped, the thigh muscle contracts, causing the lower leg to kick out.
- Neurotransmitters: These chemical messengers facilitate the transmission of impulses across synapses. For reflex arcs, neurotransmitters like acetylcholine are released at the neuromuscular junction, allowing the transmission of signals from neurons to muscles.
- Central nervous system (CNS): While many reflexes are spinal reflexes and do not involve the brain, the CNS plays a role in modulating the strength and responsiveness of these reflexes. Higher brain centers can facilitate or inhibit spinal reflexes, affecting their intensity.
Overall, reflexes represent an intricate interplay between the nervous system and the muscular system, highlighting the body’s ability to respond rapidly to stimuli for protection and coordination.
Defining What Reflex Issues Feel Like
When reflexes become abnormal, it typically indicates an underlying neurological issue. Abnormal reflexes can manifest in two primary patterns: hyperreflexia and hyporeflexia.
Hyperreflexia
This is characterized by exaggerated or overactive reflex responses. In hyperreflexia, the reflexes are more pronounced than normal. This condition often suggests an issue with the central nervous system, particularly involving the upper motor neurons.
Causes of hyperreflexia can include spinal cord injuries, stroke, brain trauma, multiple sclerosis, and other disorders that disrupt the normal inhibitory pathways of the central nervous system. In these cases, the lack of higher control leads to an increased reflex activity.
Hyporeflexia
In contrast to hyperreflexia, hyporeflexia is marked by diminished or absent reflex responses. This condition typically points to a problem in the peripheral nervous system, which includes lower motor neurons, the neuromuscular junction, or muscle fibers.
Common causes of hyporeflexia include peripheral neuropathy (as seen in diabetes), Guillain-Barré syndrome, spinal cord injuries at or below the level of the reflex arc, and muscle diseases such as muscular dystrophy. Hyporeflexia suggests a disruption in the conduction of impulses along the reflex arc pathway.
In both hyperreflexia and hyporeflexia, the abnormal reflex patterns are indicative of specific types of neural dysfunction. They are clinically significant as they provide vital clues about the location and nature of neurological problems. Medical professionals often use reflex tests as part of a neurological examination to help diagnose and monitor the progression of these disorders.
When Are Reflex Actions No Longer Normal?
Determining whether reflexes are abnormal typically involves assessing several key criteria during a neurological examination:
Reflex Grade
Reflexes are graded on a scale, usually from 0 to 4. A grade of 0 indicates no response (areflexia), 1 is a diminished or low-normal response, 2 is a normal response, 3 is brisker than normal but not necessarily indicative of a disorder, and 4 indicates a very brisk reflex, often associated with an abnormal reflex response like clonus (rhythmic oscillations following the reflex).
Symmetry
Reflexes are usually compared bilaterally. A significant difference in reflex response between the two sides of the body can indicate an abnormality. In a healthy nervous system, reflexes should be symmetrical.
Consistency
A reflex should elicit a consistent response when tested multiple times. Inconsistent responses may suggest an underlying abnormality.
A comprehensive evaluation of these factors, often alongside other diagnostic tools like imaging studies or electromyography, helps healthcare professionals determine the presence and significance of abnormal reflexes in diagnosing neurological conditions.
Accompanying Symptoms of Abnormal Reflexes
Changes in DTRs alone are not pathological, but when accompanied by other signs on examination then further investigation is needed. These associated signs and symptoms would be:
- Muscle weakness or spasticity
- Coordination issues
- Sensory disturbances
- Localized or radiating pain
- Autonomic dysfunction
- Difficulty walking
- Changes in posture
Can Cervical Radiculopathy Induce Reflex Issues?
Yes, cervical radiculopathy can indeed induce reflex issues. Cervical radiculopathy occurs when nerves in the neck (cervical spine) are compressed or irritated, often due to herniated discs, degenerative changes, or other spinal problems. This nerve compression can impact the functioning of the reflex arcs associated with the affected nerves. The specific reflex issues depend on which cervical nerve root is involved:
- Changes in reflex strength: Depending on the level of nerve root compression, there may be either a reduction or an increase in the strength of the reflex. Typically, compression leads to a diminished reflex (hyporeflexia). For example, compression of the C5 nerve root might weaken the biceps reflex, while C7 nerve root compression might affect the triceps reflex.
- Altered sensory responses: Along with changes in reflexes, cervical radiculopathy can also cause altered sensation or pain in the areas served by the affected nerve. This might be perceived as tingling, numbness, or pain in specific areas of the arm or hand.
- Muscle weakness: Compression of cervical nerve roots can lead to muscle weakness in the muscles innervated by the affected nerves, further impacting reflex responses.
- Asymmetry of reflexes: Since cervical radiculopathy often affects one side of the body more than the other, there can be asymmetry in reflex responses when comparing both sides. Learn more here: Cervical Radiculopathy: Causes, Symptoms, and Treatment
Other Medical Conditions Associated with Involuntary Reflex Action
Spinal Stenosis
Spinal stenosis is the narrowing of the central spinal canal and is a cause of significant pain and disability. Common causes of spinal stenosis include disc protrusion, facet overgrowth and ligamentum flavum thickening. Surgery is often chosen when conservative therapies fail despite the lack of convincing evidence that it is a superior treatment option. Are there alternatives to back surgery for spinal stenosis? Yes. Regenexx DDD utilizes precise platelet injections into the facets, muscles, and ligaments to treat the lumbar stenosis, treating all of the components of the issue, which is crucial. Spinal stenosis is often an age-related condition attributed…
Read More About Spinal StenosisSciatica
Disc herniation, disc protrusion, overgrowth of the facet joint, and thickening of the ligaments can result in nerve root compression or irritation, causing symptoms of sciatic compression. Some causes of sciatic compression can be interrelated with the following conditions: Degenerative disc disease, Spinal stenosis, damage or injuries to the discs, spondylolisthesis, piriformis syndrome, osteoarthritis. The symptoms of sciatica include pain in the lower back, buttock, and down your leg, numbness and weakness in low back, buttock, leg, and/or feet, pain increase with movement, “Pins and needles” feeling in your legs, toes, or feet., loss of bowel control, and incontinence. Sciatica can be treated…
Read More About SciaticaHerniated Cervical Disc
Cervical discs, also known as intervertebral discs of the cervical spine, are the specialized structures located between the vertebrae in the neck region. These discs play a crucial role in providing cushioning, flexibility, and support to the cervical spine. Structure: Cervical discs have a unique structure consisting of two main components: Nucleus Pulposus: The nucleus pulposus is the central, gel-like core of the disc. It is composed of a jelly-like substance with a high water content, giving it a soft and elastic nature. The nucleus pulposus is responsible for absorbing and distributing forces acting on…
Read More About Herniated Cervical DiscWhen to Visit a Medical Professional
Visiting a medical professional such as a physiatrist, neurologist, or even your primary care physician is needed when signs and symptoms persist and are associated with multiple other signs such as pain, weakness, numbness, or other neurologic issues.
How Do Professionals Diagnose Reflex Problems?
The diagnostic procedures for abnormal reflexes typically involve a combination of clinical assessment and supplementary tests to determine the underlying cause. Here’s an overview of the process:
- Neurological examination: The initial step usually involves a comprehensive neurological exam. This includes testing the deep tendon reflexes using a reflex hammer. The doctor assesses the reflex grade, symmetry, and consistency. They also look for pathologic reflexes (like the Babinski sign) and evaluate muscle tone and strength.
- Patient history: A detailed patient history is taken to understand any symptoms, medical conditions, past injuries, or familial diseases that might be related to the observed reflex abnormalities.
- Sensory and motor function tests: These tests assess the functioning of sensory and motor pathways. They help determine if there’s a correlation between abnormal reflexes and other neurological deficits.
- Imaging studies: Depending on the suspected cause, imaging tests like magnetic resonance imaging (MRI), computed tomography (CT), or X-rays might be performed. These tests can reveal structural abnormalities in the brain, spinal cord, or peripheral nerves that could be affecting reflex responses.
- Electromyography (EMG) and nerve conduction studies (NCS): EMG measures the electrical activity of muscles, while NCS assesses the speed and strength of signals traveling in the nerves. These tests can identify nerve or muscle damage and are particularly useful in diagnosing conditions like peripheral neuropathy or radiculopathy.
- Blood tests: In some cases, blood tests may be necessary to check for underlying conditions such as diabetes, vitamin deficiencies, or thyroid disorders, which can contribute to abnormal reflexes.
- Lumbar puncture (spinal tap): If a central nervous system infection or inflammation is suspected, a lumbar puncture may be performed to analyze the cerebrospinal fluid.
- Consultation with specialists: Referral to a neurologist or other specialists might be required for further evaluation and management, particularly if the cause of the abnormal reflexes is unclear or complex.
The combination of these diagnostic approaches allows healthcare professionals to accurately pinpoint the cause of abnormal reflexes and guide appropriate treatment. The choice of specific tests depends on the patient’s symptoms, medical history, and the findings of the initial neurological examination.
The Centeno-Schultz Approach to Managing Reflex Abnormality Issues
Treatment for abnormal reflexes largely depends on the underlying cause. Here’s an overview of various treatment options, tailored to different causes:
Physical Therapy
If the abnormal reflexes are due to conditions like nerve compression or musculoskeletal issues, physical therapy can be beneficial. Exercise and manual therapy can help improve muscle strength, flexibility, and nerve function, reducing symptoms and restoring normal reflexes.
PRP Injections
Platelet-rich plasma (PRP) injections are injectables containing blood with platelet concentrations higher than normal levels. The potential benefits of PRP injections have garnered significant interest for their simple, safe, and minimally invasive application of growth factors.
Developed at the Centeno-Schultz Clinic, Regenexx’s super concentrated PRP procedures represent an advanced form of PRP treatment. They utilize lab-processed PRP mixtures that boast 10 to 40 times higher platelet concentrations than standard PRP. Our PRP is distinguished by its elevated platelet levels, exhibiting an amber hue.
Don’t Ignore Your Symptoms; Seek Proper Treatment
Don’t ignore your symptoms or allow them to progress; seek proper medical attention for a thorough evaluation and individualized treatment plan. Your reflexes play an essential role in your body’s function and should not be taken lightly.
Trust the experts at the Centeno-Schultz Clinic for comprehensive care and optimal results. So, whether you’re experiencing abnormal reflexes or other musculoskeletal issues, let us help you get back on track to a healthier and happier life. Don’t hesitate to schedule your consultation with us today!
Don’t dismiss symptoms – they could be cervical radiculopathy. Explore more on the condition and consult our CSC specialists for a swift evaluation.