Pins And Needles In The Fingertips
A Sign Of Cervical Radiculopathy
Get Help With Feeling Of Pins And Needles In FingersAre you experiencing the sensation of pins and needles in your fingertips? This is a common symptom of cervical radiculopathy. Although many conditions can cause pins and needles, if it is accompanied by neck pain, then cervical radiculopathy would be at the top of the diagnostic list.
Cervical radiculopathy also referred to as a “pinched nerve.” is a medical syndrome that occurs when a nerve root in the neck ( cervical spine) becomes compressed or irritated leading to symptoms that include pain, numbness, tingling, and potentially weakness.
It occurs in about 85 people per 100,000 (1). Read this post to find out more about cervical radiculopathy and how it can cause pins and needles in your fingertips.
What Do Pins And Needles Feel Like?
The sensation of pins and needles may vary between different people. Here are some signs of cervical radiculopathy and how you may experience it:
- Numbness in the fingers and hands. Can be unilateral (one sided) or bilateral (both sides)
- Pain radiating along the arm and fingers
- Decreased sensation of touch
- Burning sensation in the fingers and arms
- Weakness of the fingers and arms
- Paresthesia (a prickling sensation in the fingers)
Other Symptoms Associated With Pins And Needles In The Fingers
You can also have other symptoms accompanying the pins and needles sensation that may point to cervical radiculopathy. These are:
- Cold or blue fingertips
- Neck pain
- Hypersensitivity along the arms and fingers, where even a slight touch may hurt
- Increased numbness that is directly proportional to the motor movement of the fingers during activities like writing, typing, or playing an instrument.
- Neck Pain typically one sided
- Pain with Certain movements: Pain may be aggravated by rotation, looking down or up.
- Reflex Changes: Reflexes in the affected arm may be diminished or heightened in comparison to the unaffected arm.
How Specific Positions Or Movements Can Trigger The Pins And Needles
If you are experiencing pins and needles, it’s likely that you have noticed that it can be triggered by certain movements. For example, if your symptoms are being caused by compression of a nerve, simply extending or rotating your head can trigger paresthesia and or pain. Certain movements may aggravate symptoms.
Strenuous exercises like jumping, running, lifting weights, and rolling your neck can also make the symptoms worse as it increases the strain on the cervical intervertebral discs. If these discs are damaged or bulging, the increased pressure during an intense workout can trigger the symptoms as these activities may further compress the nerve.
Additionally, positions such as sleeping on your stomach and rolling your neck can stretch already compressed nerves, thereby triggering pins and needles in your fingers or arms.
Causes Of Pins And Needles In The Fingers
There are many reasons why you may be experiencing pins and needles in your fingers. Among them are musculoskeletal causes, such as injury or carpal tunnel syndrome. Here are some of the major causes of pins and needles in the fingers:
- Herniated Cervical Disc: Sandwiched between each vertebral body is an intervertebral disc. There are 6 discs in the cervical spine. These discs are susceptible to injury and degeneration. Common injuries include disc protrusion, herniation and extrusion.
A herniated disc occurs when the intervertebral disc is forced beyond its normal margins and into the central spinal canal. This can be caused by trauma, such as an accident, or may develop over time. Sometimes, there are no symptoms.
However, since the spinal canal contains both the spinal cord and exiting nerves, the disc can irritate or compress the nerves, causing pain, pins and needles in the fingers and the arms. In severe cases, individuals may even have difficulty with normal daily activities due to pain and numbness. - Neck Injury: A traumatic or non-traumatic neck injury can damage the nerve fibers that pass through the injured region of the spine. Any injury that interrupts the nerve supply at any point along this route can cause sensory changes in the limbs, including pins and needles in the fingers.
- Osteoarthritis: There are many different forms of arthritis. The most common is osteoarthritis which is a degenerative joint disease that affects the cartilage within both large and small joints. A cervical facet joint is a small, paired joint that occurs at each level of the cervical spine.
The cervical facet joint is lined with cartilage that can be affected by osteoarthritis. Facet joints can become swollen, narrowing the boney doorway through which nerves in the neck exit. - Carpal Tunnel Syndrome: Carpal Tunnel Syndrome is a common medical condition that occurs when the median nerve, which runs through a narrow passageway called the carpal tunnel in the wrist, becomes compressed or pinched. This compression can lead to symptoms such as pain, numbness, tingling, and weakness in the hands and fingers.
The index, third and fourth fingers are most commonly affected. Carpal tunnel syndrome is often caused by repetitive hand movements, underlying medical conditions and wrist injuries. - Degenerative Disc Disease (DDD): Discs in the cervical spine are susceptible to injury and degeneration. Cervical degenerative disc disease is characterized by gradual deterioration and weakening of the discs with loss of water content and reduced ability to absorb the forces of daily living. The weakened discs can protrude or herniate irritating and or compressing the cervical nerves causing pins and needles in the fingertips.
- Cervical Spine Fracture: A cervical fracture is a potentially life-threatening injury because there are many different important structures in the neck, including nerves and blood vessels.
Cervical fractures are usually only sustained from accidents or trauma, however they can also occur with conditions such as osteoporosis or those on steroid therapy (which affects the strength of the bones). Cervical spine fractures are reported to cause 12% of all fractures with motor vehicle accidents being the most common cause followed by falls (2).
Specific cervical fractures, such as burst fractures and compression fractures, can lead to bone fragments projecting into the central spinal canal, leading to irritation or compression of the spinal cord and nerves. This can lead to a number of different neurological symptoms including pins and needles, paresthesia, or even paralysis. - Cervical Radiculopathy: Cervical radiculopathy is a medical condition that occurs when a nerve in the cervical spine (neck) becomes compressed or irritated leading to symptoms such as pain, numbness, tingling, weakness in the neck, shoulders, arms, and hand. The most common causes include herniated disc, degenerative disc disease, bone spurs, trauma and stenosis.
When a nerve in the cervical spine is pinched, the area that the nerve supplies can experience the sensation of pins and needles. - Ligament Overgrowth: Ligaments are thick pieces of connective tissue that connect bone to bone. They are susceptible to injury which in some cases can lead to thickening of the ligament.
The ligamentum flavum is an important ligament within the spinal canal that provides spinal stability. Aging, degeneration and trauma can cause this ligament to thicken. When this occurs both the central spinal canal and neural foramen can become narrowed which is called stenosis. This can lead to pins And Needles In The Fingertips. - Bone Spurs: A bone spur also known as an osteophyte is an abnormal boney growth or projection that typically forms on the edge of bones. They can develop in various part of the body that include the cervical spine. They are most often the result of instability.
Bone spurs in the neck can cause nerve irritation and compression potentially leading to pins and needles in the fingertips.
Conditions Associated With The Feeling of Pins & Needles
Bone Spurs
Bone spurs, also known as osteophytes, are bony projections that develop along the edges of bones. They are most commonly found in joints — where bones meet — but can also appear on bones where tendons, ligaments, and muscles attach. Bone spurs are often associated with aging and are a common condition. While they can occur in any bone, they’re most often found in areas such as the spine, shoulders, hands, hips, knees, and feet. Bone spurs form as the result of the body trying to repair itself by building extra bone. This process can be triggered by several factors: Osteoarthritis: The most common…
Read More About Bone SpursCarpal Tunnel Syndrome
The carpal tunnel is a tunnel-like structure in the wrist that the median nerve travels through. There are also carpal ligaments that form the roof of the tunnel and flexor tendons that also run through the tunnel. The median nerve is a branch that generates off the brachial plexus from the cervical spine in the neck. It stretches down through the arm, the wrist, and all the way into the thumb. The flexor tendons provide stability and help bend the thumb and fingers. When something causes the tunnel to narrow or the medial nerve somehow becomes compressed in the wrist, this can lead to carpal tunnel syndrome (CTS).
Read More About Carpal Tunnel SyndromeCervical Radiculopathy
Common Cervical Radiculopathy symptoms include neck pain, arm pain, shoulder pain radiating down arm to fingers, numbness, tingling, and weakness. Cervical Radiculopathy is a clinical condition in which a nerve or nerves in your neck become irritated or compressed. It is also known as ” a pinched nerve,” The causes are discussed below. It can affect individuals of any age with peak prominence between ages 40-50 years of age. Cervical Radiculopathy is due to spinal nerve inflammation, irritation, or compression. The most common causes of Cervical Radiculopathy are: Disc Injury – The disc is an important shock absorber. Unfortunately, it is susceptible to injury.
Read More About Cervical RadiculopathyHerniated Cervical Disc
Cervical discs, also known as intervertebral discs of the cervical spine, are the specialized structures located between the vertebrae in the neck region. These discs play a crucial role in providing cushioning, flexibility, and support to the cervical spine. Structure: Cervical discs have a unique structure consisting of two main components: Nucleus Pulposus: The nucleus pulposus is the central, gel-like core of the disc. It is composed of a jelly-like substance with a high water content, giving it a soft and elastic nature. The nucleus pulposus is responsible for absorbing and distributing forces acting on…
Read More About Herniated Cervical DiscPinched Nerve In Your Shoulders
If you googled “pinched nerve in shoulder,” you have come to the right place. A pinched nerve in your shoulder can not only cause excruciating pain but it can prevent the movement of your shoulder. It is important to find the cause of the pinched nerve. Is it because of shoulder pathology or cervical spinal nerves? The cause of the pinched nerve in your shoulder will dictate your treatment. We discuss the symptoms of a pinched nerve in the shoulder, the treatment options, and the alternative remedies for those who do not want invasive treatment.
Read More About Pinched Nerve In Your ShouldersRadial Nerve Palsy
The radial nerve is the largest nerve in the upper limb. It starts in the shoulder and travels through the forearm to the back of the wrist. It has nerve fibers from C5, C6, C7, C8, and T1 nerve roots. Radial nerve palsy = damage to the radial nerve which affects the muscles the nerve goes to, creating weakness in those muscles, clinically presenting with wrist drop….the inability to extend the wrist. But the radial nerve innervates many muscles of the upper arm and forearm. When injured, nerve recovery varies widely taking weeks, months, and in some cases years to recover. Addressing the underlying…
Read More About Radial Nerve PalsyThoracic Degenerative Disc Disease
Degenerative disc disease is a clinical condition that refers to the gradual deterioration of the discs located in the thoracic spine and the associated symptoms. Pain, weakness, muscle spasms, and restriction in range of motion are common. Degenerative disc disease can occur at each level of the spine: cervical, thoracic, and lumbar. Studies have demonstrated that degenerative disc disease in the thoracic spine most commonly occurs in the third to fourth decades (1) and occurs most frequently in the lower thoracic segments from T7-T12. Thoracic degenerative disc…
Read More About Thoracic Degenerative Disc DiseaseThoracic Outlet Syndrome
The thoracic outlet is an area around the collar bone where the nerves that come from your neck meet up with the blood vessels from your heart and together supply the entire upper extremity (shoulder and arm). These blood vessels (subclavian artery and vein) and nerves (brachial plexus) travel from the base of your neck to your armpit (axilla) and are considered the “thoracic outlet”. Now that you know what the thoracic outlet is, what is thoracic outlet syndrome? Simply listening to a patient’s history and completing a physical examination is all that is needed to diagnose TOS. But more involved imaging such as X-rays…
Read More About Thoracic Outlet SyndromeWrist Tendonitis
Wrist tendonitis, also known as tenosynovitis, is a condition characterized by inflammation of the tendons surrounding the wrist joint. This inflammation typically results from repetitive stress, overuse, or injury, causing the tendons to become irritated and swollen. Common contributing factors include activities that involve repetitive wrist movements, such as typing, manual labor, or sports-related motions. Additionally, sudden increases in activity level or improper ergonomics may play a role in the development of wrist tendonitis. As the tendons become inflamed, they can rub against the…
Read More About Wrist TendonitisSigns And Symptoms Of Cervical Radiculopathy By Location
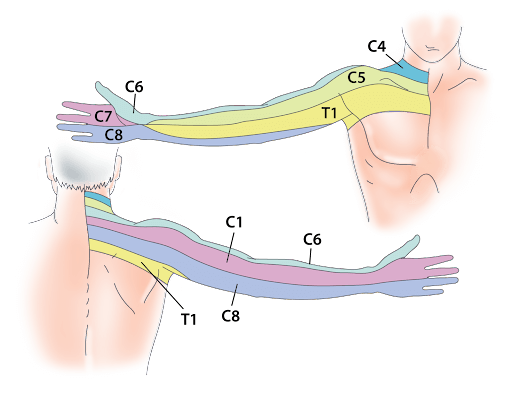
Cervical radiculopathy can cause different symptoms in various parts of the arms and hands, depending on which nerve root is affected. Here’s a list of the different cervical nerves and the radiculopathies that result due to their compression:
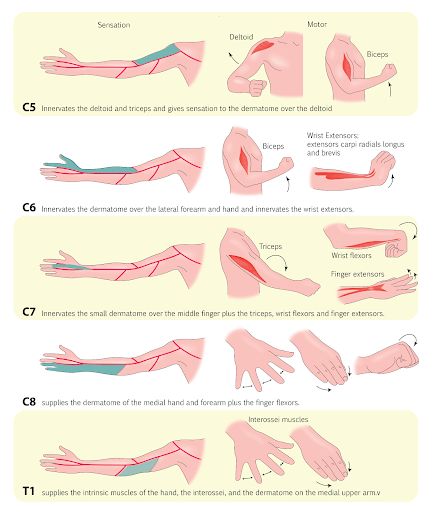
C5 Radiculopathy
C5 radiculopathy, or compression of the C5 nerve root, can affect abduction of the shoulder, where the arm cannot be lifted away from the body. This is because the C5 nerve innervates the levator scapula, rhomboid major, and minor rhomboid muscles which elevate the shoulder.
Additionally, since this nerve supplies the deltoids and biceps, people with C5 radiculopathy may experience decreased sensation, a feeling of pins and needles in fingertips, or numbness in the area over the biceps and the shoulder area.
C6 Radiculopathy
C6 radiculopathy, or compression of the C6 nerve root, can affect elbow flexion and wrist extension as this nerve root innervates the lateral arm and forearm. The muscles of the lateral arm and forearm are responsible for elbow flexion and wrist extension. Elbow flexion takes place with stimulus from a conjunction of nerves C5, C6, C7.
Compression of the C6 nerve root can lead to a loss of sensation and the feeling of pins and needles in the arm, palm, index and middle finger, and wrist.
C7 Radiculopathy
C7 radiculopathy, or compression of the C7 nerve root, can affect elbow extension and wrist flexion as this nerve root innervates the small area over the middle finger and the triceps. The triceps are responsible for elbow extension.
The sensory impairment of C7 commonly overlaps with C6 because they supply a shared area of the wrist of the middle finger and movement of the wrist and elbow. Both C6 and C7 radiculopathy can present with loss of sensation, pins and needles sensation, and altered wrist movements in this area.
C8 Radiculopathy
C8 radiculopathy affects thumb extension. It innervates the medial hand, forearm, and finger flexors. Compression of the C8 nerve root will lead to pins and needles sensation in this region and an inability to flex the fingers. The extensor digitorum, the thumb extensor, is innervated by the posterior interosseous nerve which is a branch of radial nerve coming from C7 and C8.
How Does Cervical Radiculopathy Cause Pins And Needles In The Fingers?
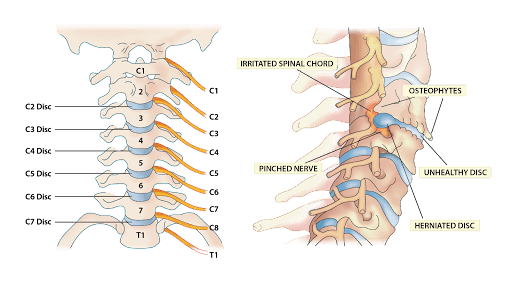
Cervical radiculopathy can cause sensory changes in the arm and forearm due to compression of one or more nerves as they exit the spine. At each level of the spine a nerve exits the spinal column through a boney doorway called the neuroforamen. The nerve then travels to a specific area such as the shoulder or forearm. Any condition that narrows the nerves pathway away from the spine can lead to nerve irritation or compression.
Common examples include cervical degenerative disc disease, disc protrusions, disc herniations and bone spurs. Nerve irritation or compression can lead to pain, pins and needles and weakness.
Neurological Deficits
A neurological deficit, also known as a neurological impairment, refers to any abnormality or impairment in the normal functioning of the nervous system. The most common neurologic areas that are affected are:
Motor Function: refers to muscle control, coordination and movement
Sensory Function: refers to ability to perceive and interpret sensory information. Examples include hot, cold, sharp, dull, wet and dry.
Reflexes: common examples include bicep, tricep and patellar reflexes which are commonly evaluated during a physical examination. Abnormal or absent reflexes can be indicative of neurologic impairments.
The chart above demonstrates how the cervical nerves supply sensation to specific areas in the arm, called dermatomes. When a nerve is irritated, injured, or compressed, it can lead to neurological deficits such as diminished or heightened sensations, motor weakness (diminished strength) , and reflex issues. The following outlines the details of the neurological deficits that can occur with nerve compression:
- Sensory Issues: There are seven cervical vertebrae with eight cervical spinal nerve roots which are labeled from C1 to C8.
These nerve roots branch off to form many different nerves, including the median nerve, ulnar nerve, and radial nerve. When these nerves are compressed, it can also lead to sensory issues, such as pain or pins and needles.
A person may also experience the sensation of their skin crawling, misinterpret hot and cold sensations, or even have a heightened response to touch. These symptoms can fluctuate depending on the extent of the compression, and are commonly exacerbated by movement. - Motor Issues: The nerve roots emerging from C5 to C8 innervate the muscles of the arm and forearm. When the nerve roots are compressed, muscle function may be affected. Over time, muscles can decrease in size and become weak.
- Reflex Issues: Compression of the cervical nerve roots can decrease the intensity or presence of these reflexes
Will The Pins And Needles In Your Fingers Resolve On Its Own?
How long the pins and needles in your fingers will last depends upon many different factors that include the duration and severity of the nerve irritation, overall nerve health, current medications, past surgical and medical history.
Pins and needles, muscle weakness and pain that do not resolve with conservative care warrants medical evaluation. Why? Persistent nerve irritation can potentially lead to permanent nerve injury with impairment in muscle strength and function.
When To Seek Medical Advice
The symptoms of pins and needles can fluctuate throughout the day, particularly after a period of rest. As a result, some people may have a false sense of recovery. However, here are some symptoms you should not ignore and require immediate medical input:
- Loss of consciousness
- Changes in sensation
- Loss of movement in the arms, such as weakness or loss of motor control
- Dizziness or fainting spells
- Altered or slurred speech
- Changes in vision
- Seizures
- Reduced balance or repeated falls
- Difficulty of breathing
- Paralysis
- Sudden or severe headaches
- Hyperdynia (heightened pain response) or allodynia (pain from a non-painful stimulus)
- Loss of bladder or bowel control
How Diagnosis Works
A doctor can diagnose the cause of pins and needles in your fingers through a stepwise approach. Here are the steps a doctor may follow:
Medical History: Your doctor will take a detailed history including any complaints of radicular pain or muscle weakness. Onset, severity, location and aggravating and alleviating factors will be identified. Also important is past medical, surgical history, medications and overall health.
Physical Exam: During the examination, your doctor will carefully evaluate your symptoms based on the location and pattern of pain, paresthesia, sensory deficits, and motor deficits. Four tests are commonly used to diagnose cervical radiculopathy: Spurling’s Test, Upper limb Tension Test, Distraction Test, and Cervical Range Of Motion (ROM) Test. When all four tests are positive, there is a 90% probability of cervical radiculopathy. The tests are listed below:
- Spurling’s Test: Spurling’s Test starts with the patient sitting down. There are variations of the test, but the most commonly used are Spurling’s Test A and Spurling’s Test B.
Patient is seated and instructed to bend their head toward the side of the symptoms. The examiner then applies downward pressure on the patient’s head. If pain, numbness, tingling or other symptoms occur, the test is positive. - Upper Limb Tension Test: The Upper Limb Tension Test assesses the median nerve. Here, the doctor depresses the patient’s shoulder, abducts the arm to 110°, and flexes the elbow 90°.
Then, the doctor externally rotates the shoulder to 90°, extends the patient’s wrist and fingers, and slowly extends the elbow. The test is positive when there is pain radiating to the fingers and arms. - Distraction Test: The patient starts by lying in supine. The doctor securely grasps the patient’s head by placing each hand behind the patient’s jaw, while standing at their head. Then, the doctor slightly flexes the patient’s neck and pulls the head towards their torso, applying a distraction force.
The test is positive when the pain or the pins and needles sensation is reduced or eliminated with traction.

- Cervical ROM Test: A Cervical ROM Test is completed to assess cervical flexion-extension, lateral flexion, and rotation with bedside instruments like a goniometer, inclinometer, and the cervical range of motion (CROM) instrument. The test is positive when the range of motion is less than 60 degrees.
Medical Testing: Several blood tests may also be necessary to find out why you may be experiencing pins and needles. These may include testing vitamin B12, lead, liver function tests, and medication levels.
Certain medications such as anti-epileptic medications, chemotherapy, HIV medications, and antibiotics can cause pins and needles. If you have been on these medications, your doctor may want to run blood tests to see if that is the cause of your symptoms.
X-Rays: An x-ray of the cervical spine may be requested by your doctor to check for fractures, disc height, and the presence of any degenerative changes, bone spurs and misalignment.
CT Scans: CT scans can provide a more detailed image of the affected area, and may be requested by your doctor to detect any bony cervical spine injuries.
MRI: An MRI is commonly used to evaluate the soft tissues in the neck which include muscles, ligaments, tendons, nerves and the spinal cord.
An MRI can identify the exact level and severity of nerve irritation or compression. In addition it can identify the causes of the irritation such as a disc herniation.
Angiogram: Cervical radiculopathy can also be caused by vertebral artery loop formations (although this is extremely rare). Angiograms are commonly used to assess these, as well as to look for an embolism in the arteries that could cause the pins and needles or numbness, alongside other symptoms.
Electromyography (EMG) : Electromyography and nerve conduction studies can confirm dysfunction of the affected nerve root. These tests evaluate the nerve roots and their conduction velocities to see how fast the nerves are conducting signals.
As the sensation of pins and needles is thought to be caused by abnormal nerve conduction, this test can determine which nerves are misfiring or not conducting effectively.
Nerve blocks: Selective nerve root blocks are also used to confirm the location of the nerve root compression and pain.
The procedure involves injecting a small amount of local anesthetic along a specific nerve root under x-ray guidance. If pain and symptoms resolve, the injected cervical level is most likely the origin of the pain.
Treatment Options For Cervical Radiculopathy
The treatment for cervical radiculopathy is usually implemented in a stepwise fashion. Depending on the cause of the symptoms, common treatments include the following:
Rest and Supportive Measures
Conservative treatment options for cervical radiculopathy include:
- Rest: Rest is essential in allowing the affected area to heal, including avoiding certain activities that may cause pain or aggravate the condition.
- Heat: Applying heat can reduce inflammation, increase blood flow, and reduce pain
Medications
When pain or dysfunction persists despite rest and heat, medications are often utilized.
- NSAIDs (nonsteroidal anti-inflammatory drugs): Over-the-counter medications such as Ibuprofen, Advil, and Naproxen can effectively relieve rib pain. These medications should be avoided as they have significant side effects.
- Oral steroids: Steroids are powerful anti-inflammatory agents that reduce swelling and pain. Common examples include Medrol dosepak, cortisone, and prednisone. Steroids have significant side effects and may make the underlying condition worse, and for these reasons should be avoided.
Therapeutic Interventions
Effective therapies to address and treat cervical radiculopathy:
- Posture improvement: Improving posture and spinal alignment can reduce thoracic spine pain and rib pain.
- Physical therapy: Physical therapy can help to strengthen the muscles around the affected area, improve flexibility, and alleviate pain.
- Chiropractic care: Chiropractic adjustments can help to realign the rib and surrounding structures, which may help alleviate pain.
Invasive Interventions
When conservative care and oral medications fail, patients are often referred for injections. Unfortunately, not all injections are the same. The most common injections are steroids, which are offered by pain clinics.
- Steroid injections: Steroids are powerful anti-inflammatory agents that reduce inflammation. They are utilized in an attempt to reduce pain and improve function. Cervical epidural steroid injections are the most common treatment for cervical radiculopathy. There are two major types of cervical epidural steroid injections: interlaminar and transforaminal. The difference is critical and patients need to specifically ask which procedure is recommended.
Steroids have significant risks that include injuring the ligaments, joints, muscles, and discs in the spine and should be avoided. Steroids have been demonstrated to injure joint cartilage.(6)
PRP: Your Best Treatment Option
At the Centeno Schultz Clinic we offer the evaluation of patients with ongoing neck pain, dysfunction and pins and needles by board certified, fellowship trained physicians. Evaluations include medical history, physical examination and review of imaging.
PRP is an effective treatment option for cervical radiculopathy as it allows patients to use their own blood to accelerate healing and repair.
Alternative to Steroid Injections
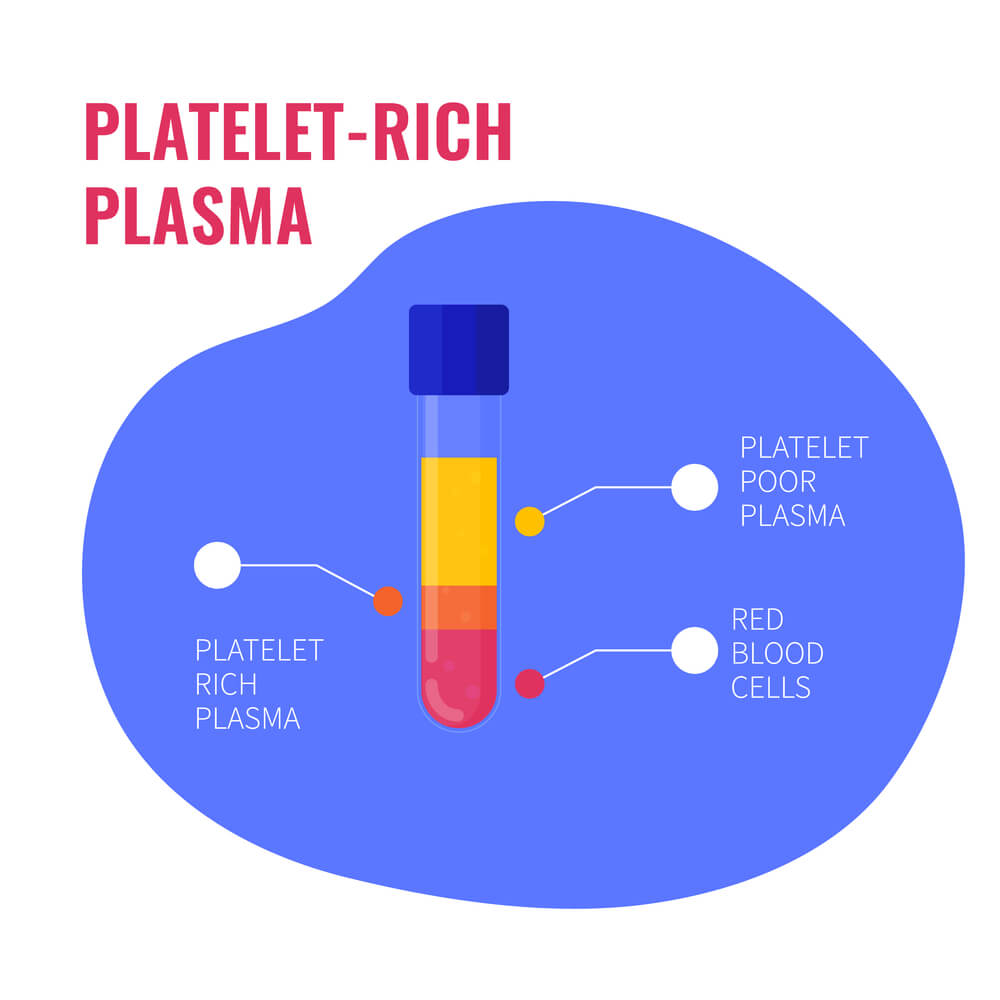
PRP is an effective alternative to cervical steroid injections for the treatment of cervical radiculopathy. PRP is a type of regenerative medicine treatment that involves using a patient’s own blood to stimulate healing and tissue repair. The are 3 principal steps:
- Blood collection: blood is drawn from into vials similar to a routine blood test.
- Centrifugation: A method of separating the platelets from the other parts of the blood such as the plasma and red blood cells. It works by spinning the blood and because of the different particle densities the blood separates into different layers. In most clinics this is performed by a bedside centrifuge.
- Injection: The concentrated platelets are then injected into the area of tissue damage.

PRP is rich in a large number of growth factors that can increase blood flow and decrease inflammation.
Are All PRP Treatments the Same?
No! Not all PRP injections are the same. At the Centeno Schultz Clinic we have 17 years of experience in the use of PRP and other orthobiolgic treatments. We have published extensively in the field of PRP and bone marrow concentrate. Important differences include:
- Concentration: The concentration of the PRP makes a difference as the patients older than 30 years of age require a higher dose of prp than younger patients. Bedside centrifuges do not offer the flexibility of different PRP concentrations. Most provide only low concentration PRP. At the Centeno-schultz Clinic we have a university based laboratory with a flexible platform that allows us to customize all PRP injections from 3x -20x.
- Injection: Unfortunately there is a wide range of skills and techniques in those offering PRP treatments. Some clinics utilize mid level practitioners that perform pRP injections without any guidance.
At the Centeno-Schultz Clinic all providers are board certified, fellowship trained physicians who have years of advanced training. All injections are performed with x-ray and or ultrasound guidance. Why? To ensure that the PRP is injected into the area of injury or damage. This ensures the best clinical outcome. - Treatment Plans: Most clinics offer simple injections. At the Centeno-Schultz Clinic we acknowledge that the human body has many different moving parts that work together. This concept is referred to as the functional spine unit. Our treatment plans are inclusive and address the many different parts of the spine. Examples include evaluating and treating the cervical nerve root, facet joint, ligaments, fascia and tendons. The comprehensive approach provides for the best clinical outcomes.
Don’t Underestimate The Sensation Of Pins And Needles
If you have pins and needles in your arm and fingers, do not underestimate them. Seek medical help immediately so that your nerves can be evaluated without delay. If not, the damage to your nerves could be permanent.
A doctor will be able to accurately diagnose your symptoms based on your history, a physical examination, and imaging (when necessary). With the correct diagnosis, your doctor will be able to recommend the most suitable treatments to help resolve your symptoms, including PRP if you are a good candidate.
PRP is one of the best treatment options for cervical radiculopathy and has few risks and side effects when compared with surgical interventions.
Are you experiencing pins and needles in your fingertips? Learn more about cervical radiculopathy here or book consult with our doctor to find out the cause of your symptoms.
References:
- Schoenfeld AJ, George AA, Bader JO, et al. Incidence and epidemiology of cervical radiculopathy in the united states military: 2000 to 2009. J Spinal Disord Tech. 2012; 25:17–22. doi: 10.1097/BSD.0b013e31820d77ea.
- Yadollahi M, Paydar S, Ghaem H, et al. Epidemiology of Cervical Spine Fractures. Trauma Mon. 2016;21(3):e33608. Published 2016 Mar 16. doi:10.5812/traumamon.33608
- Nordin M, Randhawa K, Torres P, Yu H, Haldeman S, Brady O, Côté P, Torres C, Modic M, Mullerpatan R, Cedraschi C, Chou R, Acaroğlu E, Hurwitz EL, Lemeunier N, Dudler J, Taylor-Vaisey A, Sönmez E. The Global Spine Care Initiative: a systematic review for the assessment of spine-related complaints in populations with limited resources and in low- and middle-income communities. Eur Spine J. 2018 Sep;27(Suppl 6):816-827.
- Takeuchi M, Wakao N, Hirasawa A, et al. Ultrasonography has a diagnostic value in the assessment of cervical radiculopathy: A prospective pilot study. Eur Radiol. 2017;27(8):3467-3473. doi:10.1007/s00330-016-4704-9
- Lam KHS, Hung CY, Wu TJ. Ultrasound-Guided Cervical Intradiscal Injection with Platelet-Rich Plasma with Fluoroscopic Validation for the Treatment of Cervical Discogenic Pain: A Case Presentation and Technical Illustration. J Pain Res. 2020; 13:2125-2129. Published 2020 Aug 20. doi:10.2147/JPR.S264033