How to Avoid Knee Replacement: A Quickstart Guide
Am I a Candidate?Your knee pain initially was intermittent and mild. Unfortunately, It is now constant and debilitating. Your doctor recommends knee replacement surgery. What is the knee composed of? What are the most common knee injuries? What is knee replacement surgery? What are the different types of knee replacements? What is knee replacement surgery success? What are the 12 most common complications associated with knee replacement surgery? What regenerative treatment options exist? How to avoid knee replacement? Let’s dig in.
Knee Basics 101
The knee is an important joint compromised of bones, muscles, ligaments, tendons, cartilage, and meniscus.
Bones: The femur (thigh bone) connects with your tibia (shin) to form the knee joint. The ends of both bones are covered with cartilage which allows for smooth, painless movement of the knee.
Muscles: There is an extensive number of muscles that move and stabilize the knee joint. Common examples include the quadriceps (located on the front of the thigh) and hamstrings (located on the back of the thigh).
Ligaments: Thick pieces of connective tissue that connect bone to bone. They provide critical stability for the knee. A common example is the Anterior Cruciate Ligament (ACL).
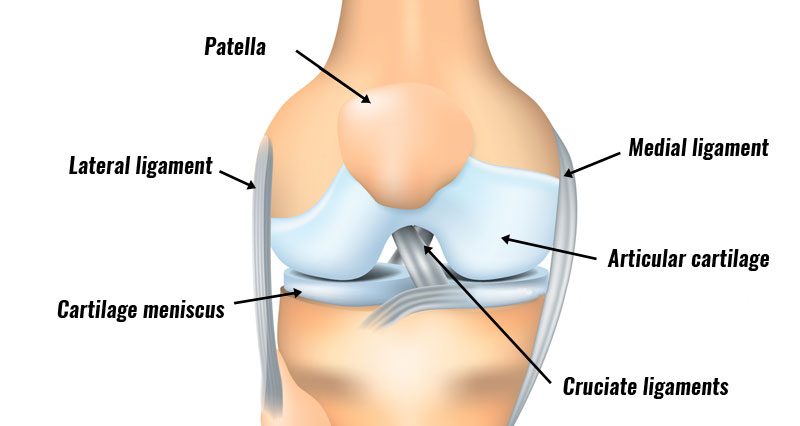
Tendons: Thick pieces of connective tissue that connect muscle to bone. Tendons provide important stability and strength. A common example is a patellar tendon.
Meniscus: A C-shaped piece of fibrocartilage sandwiched between the thigh bone and shin bone. It functions as a shock absorber. There are two menisci per knee: one on the inside also referred to as medial and one on the outside of the knee (lateral).
Knee Injuries
Knee injuries are very common and increasing in number. An estimated 6,664,324 knee injuries presented to US Emergency Rooms from 1999 through 2008, for a rate of 2.29 knee injuries per 1,000 population (1). Patients between 15 to 24 years of age had the highest injury rate. Individuals with a history of knee injury are 3 to 6 times more likely to develop knee osteoarthritis (2,3).
Common injuries include:
Sprain
A sprain is the stretching or tearing of a ligament. A common example is an injury of the MCL in the knee.
Strain
A strain is the stretching or tearing of a muscle. A common example is a hamstring strain after running.
Lacerations/punctures
Trauma can a tear or abrasions in the skin which if left untreated can cause infection.
Meniscus tears
The meniscus is susceptible to injury and can be torn. There are many different types of tears that are classified based on location, severity, and pattern.
Fractures
A fracture is when the bone breaks. There are different types of fractures which include.
A displaced fracture is when the bone breaks into two or more pieces and moves out of alignment.
A non-displaced occurs when the bone breaks but does not move out of alignment.
A closed fracture is when the skin is not broken.
An open fracture occurs when the bone rips open the skin and is visible.
Arthritis
Arthritis is inflammation of the knee joint resulting in pain, swelling, and stiffness. Many different types of arthritis with osteoarthritis being the most common. Osteoarthritis, also known as wear and tear arthritis is a condition where the cartilage wears down over time.
Want to Get Back to What You Love, Without Surgery and Medication?
What Is Knee Replacement Surgery?
Knee replacement surgery, also known as knee arthroplasty, is a major surgery where the actual joint is surgically amputated and replaced with an artificial joint. The procedure is performed in a hospital or ambulatory surgery setting with general anesthesia or spinal block. The indication for knee replacement surgery is growing and includes severe knee pain, limited activity, persistent inflammation, restricted range of motion, and mechanical misalignment (4).
Are there Different Types of Knee Replacements?
There are three major types of knee replacement.
Total Knee Replacement
A total knee replacement involves the complete replacement of the knee with an artificial joint.
Partial Knee Replacement
A partial replacement involves replacing only a portion of the joint. Typically the inside (medial) or outside (lateral) aspect of the joint is replaced.
Knee Cap Replacement
A knee cap replacement involves the removal and replacement of just the kneecap.
What Is Knee Replacement Success?
The best study to date performed on knee replacement is a 2015 RCT that compared knee replacement to physical therapy (5). 100 patients with moderate to severe knee osteoarthritis were randomized to undergo total knee replacement, or, 12 weeks of conservative treatment including PT, exercises, and diet modification. Here are the results.
- 3 in 4 patients in the physical therapy group decided not to get a knee replacement
- About half of the knee replacement group reported some sort of serious complication
- While the knee replacement group had better functional improvement than physical therapy in some tests, in others there was no difference
- You needed to perform 6 knee replacements before one person reported that they had at least 15% better function. This is called an NTT of 6. NTT stands for the number needed to treat.
To learn more about this study and what NTT is please click on the video below.
The 12 Most Common Complications Associated with Knee Replacement Surgery
Knee Replacement Surgery is major surgery. Based on the advertising and the quickness with which knee replacment is recommended, you may be wondering why we would be writing about how to avoid knee replacement. Knee replacement has many significant risks and complications. The 12 most common include:
1. Persistent Knee Pain
A large systemic review of many studies reviewed the results of 14 studies that reported pain after knee replacement surgery. That study demonstrated that between 10% to 34% of patients reported chronic pain despite getting their knees replaced (6).
2. Patient Dissatisfaction
Another large study looked at 1217 consecutive patients who had knee replacements between 2006 and 2008 and who filled out the validated quality of life and functional questionnaires. The result? 1 in 5 people were dissatisfied with their knee replacement results (7).
3. Replacement Joints Wear Out Requiring Additional Surgery
Artificial knee joints do not last forever. The younger you are at the time of the knee replacement the more likely you will wear out the artificial joint (8). This most often requiring additional surgery. The risks of your knee replacement wearing out increase if you are overweight, do heavy manual labor, run, or play vigorous sports.
4. Deep Vein Thrombosis ( DVT)
DVT is is a serious medical condition in which a blood clot forms in one or more of the deep veins in your body. This typically occurs in the legs. The blood clot can travel through the bloodstream into the lungs causing blockage of blood flow. This is called a pulmonary embolism. 3% of DVT cases are reported during the hospital stay.
5. Infection
Infection is a serious condition and may involve the skin, muscles, or artificial joint. Antibiotics are often required. If the infection involves the bone antibiotics are given intravenously over several weeks. In severe cases, the artificial joint must be surgically removed and replaced at a later date after the infection has resolved.
6. Artificial Joint Becomes Loose or Dislocates
After your ” arthritic” knee is surgically amputated, the artificial joint is inserted and cemented into place. Unfortunately, the cement does not always hold. The result is an artificial joint that becomes loose or dislocated. The treatment often requires another surgery.
7. Allergic Reactions
Artificial knee joints may contain titanium or a cobalt-chromium-based alloy. The bone cement is a composite epoxy. Patients can be allergic to the prosthesis, the cement, or both. Additional surgery is often required.
8. Nerve Damage
Nerve damage can and does occur during knee replacement surgery. It is estimated to occur in up to 10% of cases. Common symptoms include numbness, foot drop, weakness, tingling, burning or prickling sensation.
9. Damage to Tendons and Ligaments
Tendons are thick pieces of connective tissue that connect muscle to bone. Ligaments are connective tissue that connects bone to bone. Ligaments and tendons provide important stability for the knee. These can be injured during surgery causing pain, restriction in movement, and instability.
10. Knee Stiffness and Loss of Motion
Many patients after knee replacement complain of knee stiffness and loss of motion. Both of which limit activities like walking and playing sports.
11. Increased Risk of a Heart Attack
Knee replacement patients are 9 times more likely to have a heart attack (9)
12. A Buildup of Toxic Metal Ions in the Blood
Knee prostheses are composed of metals which with wear and tear can leak into the blood creating illness (10).
Regenerative Treatment Options
Regenerative treatment options include PRP bone marrow concentrate injections. There is high-quality literature that demonstrates the effectiveness of regenerative treatments. Specifically, there are three randomized controlled trials on using precise injections of your own bone marrow concnetrate which contains stem cells to help your arthritic knees (11-13). These now show that there is a 1 in 5 failure rate at 15 years causing those patients to convert to knee replacement. At the Centeno-Schultz Clinic, we have been treating knee injuries over the last 16 years with PRP and bone marrow concentrate injections. Our results speak for themselves and are available here. We have also published our results in an effort to advance the field of interventional orthopedics.
How To Avoid Knee Replacement Surgery
Knee replacement surgery is a major surgery associated with significant risk and complications. 5 steps on how to avoid knee replacement surgery and still accomplish your goals.
Address the Little Problems Before they Progress
Orthopedic conditions are progressive in nature and typically get worse over time. When a problem or pain arises that does not respond to rest and conservative care, acknowledge it and get it evaluated and treated.
Maximize Conservative Care
Explore and utilize conservative care. Surgery is a one-way street: there is no turning back.
Take a Comprehensive Approach
The body is a complex, interwoven unit. Look beyond the given joint that is currently problematic. For example, all patients with knee pain should have their ankles, hips and low back evaluated as they all play an important role in knee function and performance.
Understand the Source of your Pain and Limitation
The knee is compromised of many different parts which were discussed above. Each can cause pain and limitation. Don’t accept the claim that it is arthritis or a tear in your meniscus that is causing your pain. Schedule an in-office or virtual evaluation at the Centeno-Schultz Clinic and learn what is actually causing your knee pain and dysfunction.
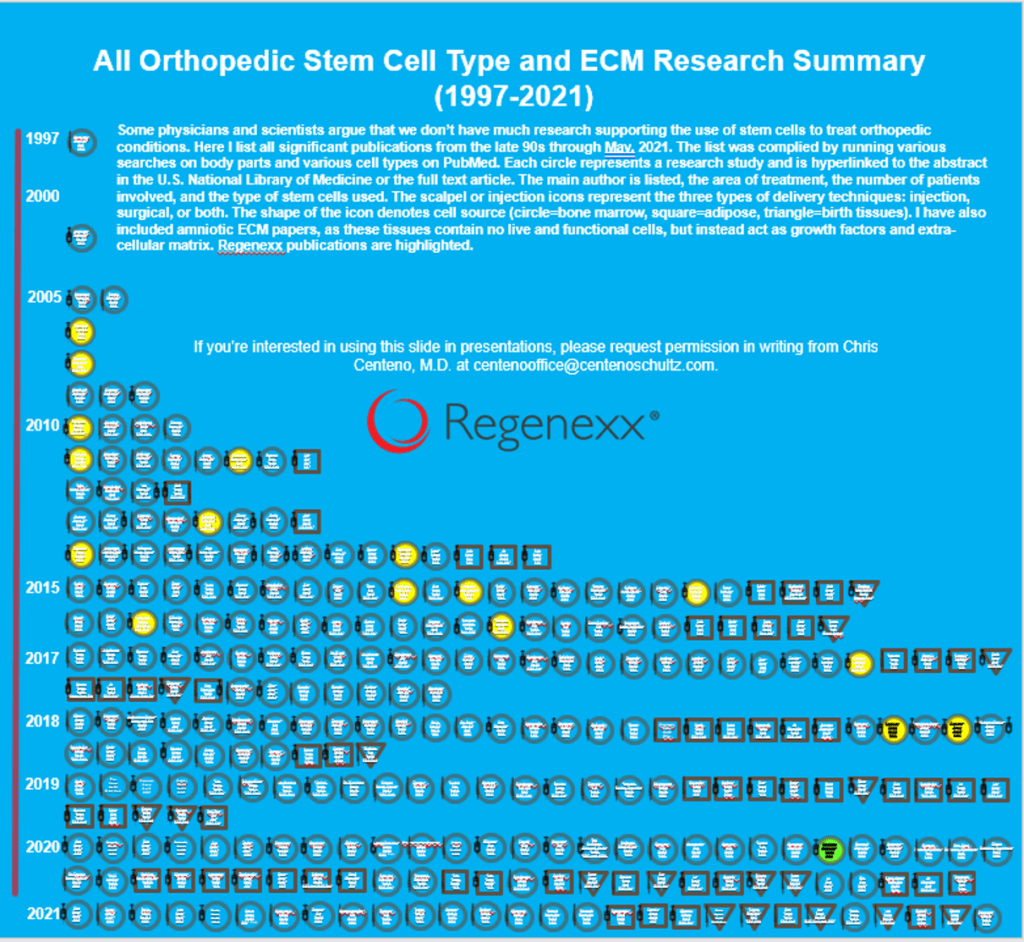
Embrace Regenerative Treatment Options
Naysayers claim that is literature to support the use of stem cells for orthopedic conditions. Nothing could be further from the truth. Compiled below is a summary of all the stem cell publications from the late 90’s through May 2021. The list is compiled by running various searches on body parts and various cell types on Pub Med.
In Conclusion
- The knee is composed of bones, muscles, ligaments, tendons, cartilage, and meniscus.
- Knee injuries are common and are increasing in number.
- Common knee injuries include sprain, strain, lacerations, meniscus tears, fractures, and arthritis.
- Knee replacement surgery, also known as knee arthroplasty is a major surgery where the actual joint is surgically amputated and replaced with an artificial joint.
- There are three different types of knee replacement surgeries: Total knee, partial knee, and knee cap replacement.
- A 2015 randomized controlled study compared knee replacement surgery to physical therapy with surprising results.
- The 12 most common complications associated with knee replacement surgery include persistent knee pain, patient dissatisfaction, deep vein thrombosis, infection, wearing out of artificial joint, allergic reactions, nerve damage, tendon and ligament damage, knee stiffness, increased risk of heart attack, and toxic metal ions in the blood.
- Regenerative treatment options include the use of PRP and bone marrow concentrate.
- Three high-level randomized controlled trials exist that use precise injections of bone marrow concentrated to help arthritic knees.
5 Ways to Avoid Knee Replacement Surgery
Address the Little Problems before they Progress
Maximize Conservative Care
Take a Comprehensive Approach
Understand the Source of your Pain and Limitation
Embrace Regenerative Treatment Options. Learn about our regenerative knee surgery alternatives.
If you are committed to living a life without dependence on additive medication or the risks associated with knee replacement the good news is you have options on how to avoid knee replacement. To learn if you are a candidate for stem cell or PRP treatments. Speak with a board-certified, fellowship-trained physician who will review your history, imaging, and provide you with a candidacy rating. Schedule an in-office evaluation or telemedicine visit. Knee pain if left untreated gets worse. Act now before it is too late.
- Gage BE, McIlvain NM, Collins CL, Fields SK, Comstock RD. Epidemiology of 6.6 million knee injuries presenting to United States emergency departments from 1999 through 2008. Acad Emerg Med. 2012 Apr;19(4):378-85. doi: 10.1111/j.1553-2712.2012.01315.x. PMID: 22506941.
- Muthuri SG, McWilliams DF, Doherty M, Zhang W. History of knee injuries and knee osteoarthritis: a meta-analysis of observational studies. Osteoarthritis Cartilage. 2011 Nov;19(11):1286-93. doi: 10.1016/j.joca.2011.07.015. Epub 2011 Aug 16. PMID: 21884811.
- Felson DT, Zhang Y. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum. 1998 Aug;41(8):1343-55. doi: 10.1002/1529-0131(199808)41:8<1343::AID-ART3>3.0.CO;2-9. PMID: 9704632.
- Gademan MG, Hofstede SN, Vliet Vlieland TP, Nelissen RG, Marang-van de Mheen PJ. Indication criteria for total hip or knee arthroplasty in osteoarthritis: a state-of-the-science overview. BMC Musculoskelet Disord. 2016;17(1):463. Published 2016 Nov 9. doi:10.1186/s12891-016-1325-z
- Skou ST, Roos EM, Laursen MB, Rathleff MS, Arendt-Nielsen L, Simonsen O, Rasmussen S. A Randomized, Controlled Trial of Total Knee Replacement. N Engl J Med. 2015 Oct 22;373(17):1597-606. doi: 10.1056/NEJMoa1505467
- Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012 Feb 22;2(1):e000435. doi: 10.1136/bmjopen-2011-000435. PMID: 22357571; PMCID: PMC3289991.
- Scott CE, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br. 2010 Sep;92(9):1253-8. doi: 10.1302/0301-620X.92B9.24394. PMID: 20798443.
- Valdes AM, Doherty SA, Zhang W, Muir KR, Maciewicz RA, Doherty M. Inverse relationship between preoperative radiographic severity and postoperative pain in patients with osteoarthritis who have undergone total joint arthroplasty. Semin Arthritis Rheum. 2012 Feb;41(4):568-75. doi: 10.1016/j.semarthrit.2011.07.002. Epub 2011 Aug 24. PMID: 21868060.
- Lu N, Misra D, Neogi T, Choi HK, Zhang Y. Total joint arthroplasty and the risk of myocardial infarction: a general population, propensity score-matched cohort study. Arthritis Rheumatol. 2015;67(10):2771–2779. doi: 10.1002/art.39246.
- Savarino L, Tigani D, Greco M, Baldini N, Giunti A. The potential role of metal ion release as a marker of loosening in patients with total knee replacement: a cohort study. J Bone Joint Surg Br. 2010 May;92(5):634-8. doi: 10.1302/0301-620X.92B5.23452.
- Centeno C, Sheinkop M, Dodson E, Stemper I, Williams C, Hyzy M, Ichim T, Freeman M. A specific protocol of autologous bone marrow concentrate and platelet products versus exercise therapy for symptomatic knee osteoarthritis: a randomized controlled trial with 2 year follow-up. J Transl Med. 2018 Dec 13;16(1):355. doi: 10.1186/s12967-018-1736-8. PMID: 30545387; PMCID: PMC6293635.
- Hernigou P, Bouthors C, Bastard C, Flouzat Lachaniette CH, Rouard H, Dubory A. Subchondral bone or intra-articular injection of bone marrow concentrate mesenchymal stem cells in bilateral knee osteoarthritis: what better postpone knee arthroplasty at fifteen years? A randomized study. Int Orthop. 2020 Jul 2. doi: 10.1007/s00264-020-04687-7. Epub ahead of print. PMID: 32617651.
- Hernigou P, Delambre J, Quiennec S, Poignard A. Human bone marrow mesenchymal stem cell injection in subchondral lesions of knee osteoarthritis: a prospective randomized study versus contralateral arthroplasty at a mean fifteen year follow-up. Int Orthop. 2020 Apr 23. doi: 10.1007/s00264-020-04571-4. Epub ahead of print. PMID: 32322943.
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.