Concussion headaches often occur after traumatic brain injuries. They can result from mechanical impacts and chemical changes in the brain. These headaches can cause persistent pain, sensitivity to light, and cognitive issues. It is important to accurately diagnose them to distinguish them from other types, like migraines or tension-type headaches.
If untreated, they may lead to chronic post-concussion syndrome (PCS). This condition is estimated to affect up to 43% of people who suffer a concussion, prolonging symptoms beyond the typical three-month recovery. This can severely impact daily life and cause ongoing issues with cognitive function, emotional health, and physical well-being—ultimately getting in the way of work, studying, hobbies, and participating in social activities.
In our experience, many patients who get diagnosed with post-concussion syndrome actually have an upper neck injury. One common upper neck injury type is instability, where the ligaments that hold the head on have become injured. This is called craniocervical instability or CCI.
Given the impact of untreated concussions and CCI, prioritizing an accurate diagnosis for headache sufferers is essential. The Centeno-Schultz Clinic approach, which uses dynamic imaging like digital motion X-ray (DMX), helps improve the accuracy of cranio-cervical instability diagnoses by identifying different types of instabilities in the upper cervical spine.
This whole-person strategy aids in managing or performing procedures to fix concussion-induced headaches, supporting recovery.
Understanding What Can Happen During a Concussion
A concussion occurs when an impact or forceful motion causes the brain to move rapidly within the skull. This movement might result from a direct hit, like in sports, or even from a rapid acceleration, such as a car accident.
The brain floats in cerebrospinal fluid. When the head experiences trauma, the brain collides with the skull, leading to potential bruising (contusions) and tiny injuries to the brain tissue. This impact disrupts normal brain function.
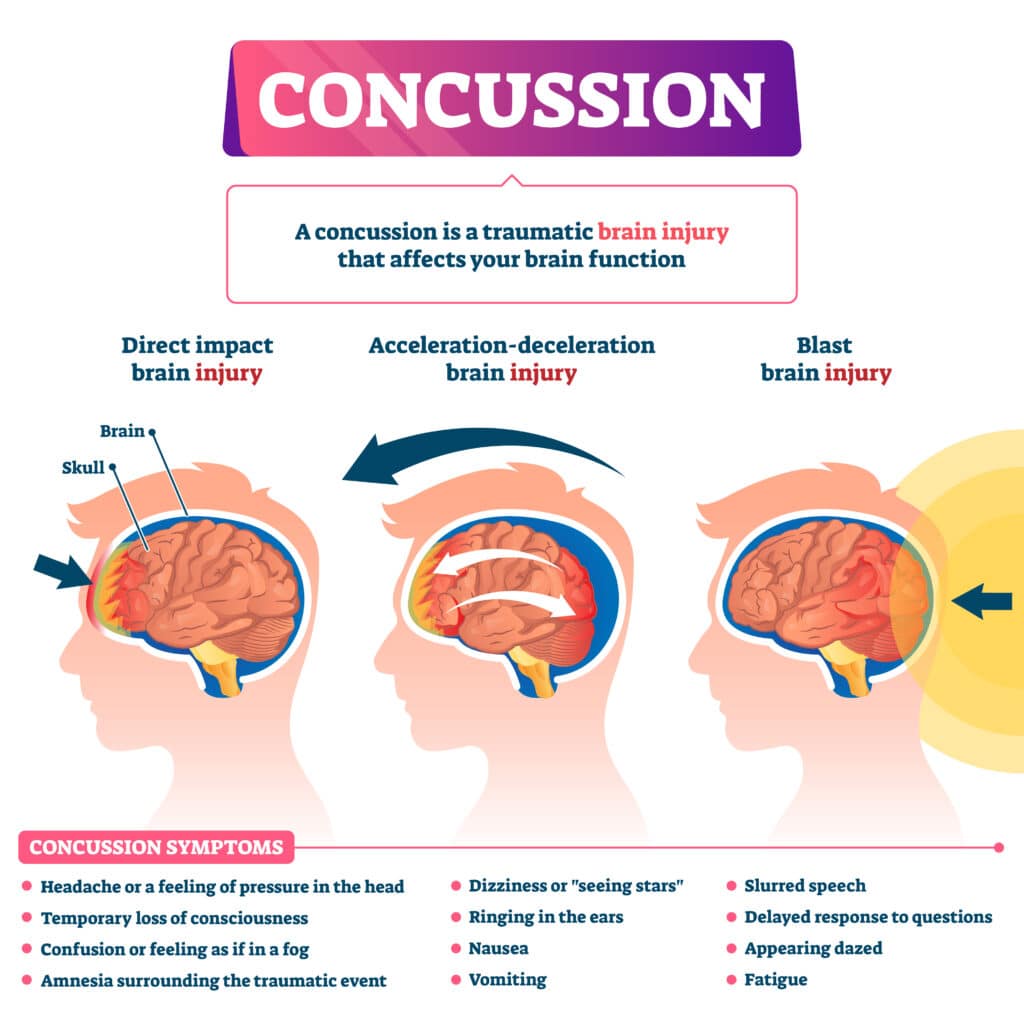
Less obvious causes include falls or repeated minor head impacts, which can accumulate over time.
Several processes and reactions take place in and around the brain following head trauma. These include:
- Axonal shearing: Rapid movement can stretch and damage brain nerve fibers (axons), disrupting cell communication, known as axonal shearing. Axonal damage can lead to cognitive issues and prolonged symptoms.
- Chemical changes: There is a sudden release of neurotransmitters and changes in ion balances within the brain cells. This can disrupt the brain’s ability to send clear signals, contributing to confusion and headaches.
- Reduction in blood flow: Blood flow to specific regions of the brain may be reduced, which can further impair brain function.
- Inflammatory response and swelling: The body’s immune response triggers inflammation in the brain, which can worsen symptoms like pain and bruising. In particular, in response to injury, the brain may swell. Swelling increases pressure within the skull, creating further complications like intense headaches or vision changes.
- Symptom onset: Symptoms such as headaches, dizziness, confusion, and cognitive issues may arise following a concussion. This is usually a consequence of the fact that the physical and chemical reactions seen above impair cell function.
- Cervical involvement: The force from the concussion can also affect the cervical spine, leading to instability, particularly in the upper cervical region. This instability can contribute to headaches and other symptoms.
- Neck ligament strain: The ligaments in the neck may be strained or damaged during the impact, which can add to the discomfort and mobility issues.
Are Headaches Usual Symptoms of Head Trauma?
Headaches are often the most immediate symptom following a concussion. Studies indicate that this symptom occurs in up to 90% of cases soon after a TBI. Post-traumatic headache symptoms can resolve within three months for some, while others experience them chronically. These studies show that around 30% of patients report persistent post-traumatic headaches after six months, and up to 58% continue after a year.
It is important not to overlook this symptom or confuse it with other, less severe types of headaches. The initial impact on the head can disrupt the brain’s functions, leading directly to increased pain sensitivity. These headaches indicate the body’s response to an injury that requires careful management.
Understanding the types and causes of these headaches helps in tailoring the right recovery plan.
Types of Headaches Associated with Concussions
Concussions can manifest several types of headaches:
- Tension-type headaches
Tension-type headaches can result from head or neck trauma when muscles in these areas tighten due to stress or strain. Damage to nearby structures, like broken bones or strained ligaments, can cause changes in the posture’s alignment, causing additional stress and tension headaches.
Symptoms include a dull, achy sensation across the forehead or back of the head, often described as a tightening band. Poor posture or jaw clenching post-concussion can exacerbate these headaches.
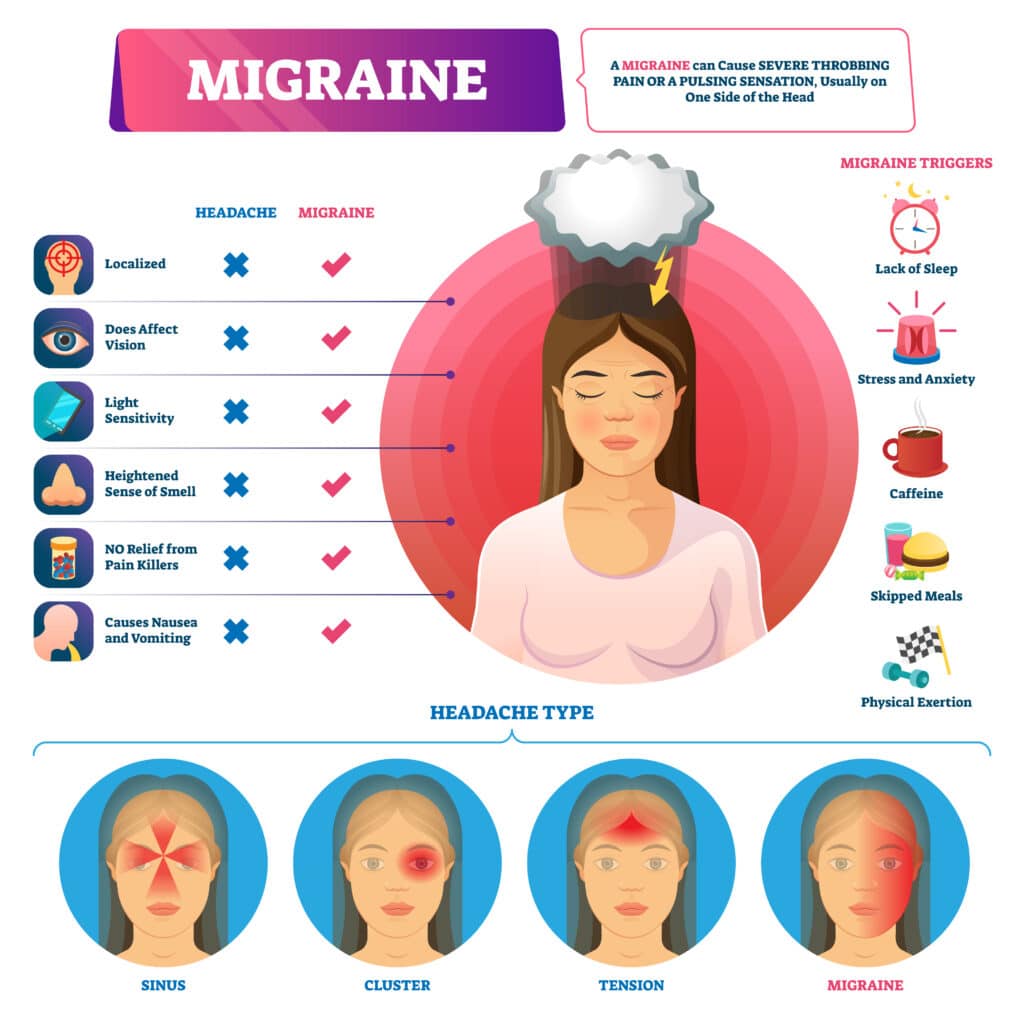
- Migraines
Migraines are a distinct type of headache caused by changes in the electrical activity in the brain. They differ from other headaches in their intensity and symptoms, which often include severe, throbbing pain on one side of the head, accompanied by nausea, light sensitivity, or visual disturbances like flashing lights.
Following a concussion, migraines can occur due to changes in the brain’s electrical activity post-injury. Factors such as stress, dehydration, and sleep disturbances, which often worsen after a concussion, can trigger these migraines. A 2023 study also concluded that TBI patients had a higher risk of suffering from migraines compared to those without a concussion.
- Post-traumatic headaches
Post-traumatic headaches share characteristics with both tension-type headaches and migraines. They typically develop within seven days after a head injury. Symptoms may include constant, throbbing pain that might fluctuate in intensity. These headaches are believed to be a direct consequence of the injury to brain tissues, which results in biochemical changes and inflammation. They may persist well into the recovery phase.
- Cervicogenic headaches
Cervicogenic headaches originate from issues in the cervical spine and neck, usually due to whiplash motion or direct injury to the neck during the concussion. They are frequently confused with tension headaches, but a key difference is that neck movement will trigger pain in cervicogenic headaches. Symptoms often include pain that starts at the back of the head and radiates towards the forehead, along with restricted neck movement.
Common Causes of Concussion Headaches
Understanding the cause of concussion headaches is essential for effective treatment and management.
- Brain injury: After a brain injury, neurotransmitter levels become unbalanced, making the brain more sensitive to pain signals. This can lead to increased head pain. Additionally, the body’s response to the injury includes inflammation, which causes swelling and further amplifies pain sensations. These two factors—neurotransmitter imbalance and inflammation—combine to cause the post-injury head pain often experienced after a concussion.
- Increased pressure in the brain: After a concussion, the brain may swell. Swelling results from an inflammatory response as the body attempts to heal damaged brain tissues. When the brain swells, the pressure inside the skull (intracranial pressure) increases. This pressure can compress brain tissues and disrupt normal function. Symptoms may include pain and confusion. In severe cases, swelling can cause serious complications such as reduced blood flow, brain damage, or life-threatening conditions.
- Neck and spinal injury: A concussion often involves an abrupt movement of the head and neck, potentially resulting in injuries to soft tissues like cartilage or ligament tears. These injuries can radiate pain upwards to the head, causing headaches. Neck strain might also disrupt sleep patterns and daily activities, increasing the risk of headaches.
- Stress and anxiety: Mental stress and anxiety frequently accompany concussions. This psychological distress can increase muscle tension and activate the pain pathways in the brain. These reactions can result in frequent, more intense headaches.
A comprehensive approach to recovery should take into account psychological factors. Stress-management techniques, such as relaxation exercises and cognitive-behavioral therapy, may help improve mental health, which plays a role in helping traumatic brain injury patients recover.
Why Constant Concussion Headaches May Be Linked to Underlying Conditions
Concussion headaches should ease down within weeks as the damaged tissues recover and inflammation subsides. However, in some cases, symptoms like headaches and tension can persist beyond the typical recovery period of three months. When this occurs, these symptoms are considered chronic, and they may hint at an underlying condition.
Persistent headaches can result from:
- Brain changes post-injury: These changes might involve structural shifts or biochemical alterations that disrupt normal brain function.
- Inflammation: Inflammation can aggravate headache symptoms by increasing pressure in the skull.
- Damaged upper neck facet joints: These joints are between your head and neck and are frequently injured during a concussion. Sometimes, they heal on their own, and sometimes, they don’t heal, causing pain that is felt in the head.
- Nerve irritation: If the nerves in the cervical spine become irritated or damaged, patients may experience headaches. These nerves, such as the greater and lesser occipital nerves, refer pain and symptoms to the head.
The cervical spine is often involved during a concussion or other traumatic brain injury. The neck can become strained or misaligned, worsening headache symptoms by interfering with natural nerve pathways. Addressing the neck, along with focusing on the direct brain injury, contributes to a much more comprehensive approach to recovery.
Post-Concussion Syndrome
PCS occurs when symptoms persist long after the initial injury has healed. This condition suggests more complex underlying issues within the brain. Symptoms can include:
- Persistent headaches
- Dizziness
- Difficulty concentrating
- Sleep disturbances
- Memory problems
- Sensitivity to noise and light
- Fatigue
- Irritability
- Anxiety or depression
These ongoing issues can be due to lasting structural or chemical changes in the brain, such as neurotransmitter imbalances or ongoing inflammation. It is important to identify PCS early to guide treatment strategies aimed at restoring balance to brain chemistry and function.
Upper Cervical Injuries
Injuries to the upper neck can exacerbate or fully cause headache symptoms after a concussion. Here are some mechanisms by which neck injuries contribute to headaches:
- Ligament problems: Damage to neck ligaments can lead to instability, contributing to discomfort and headaches.
- Nerve irritation: Irritated nerves in the neck can send pain signals to the head, worsening headache symptoms.
- Neck misalignment: Misalignment in the cervical spine can influence head posture and increase headache frequency.
Addressing neck irritation and alignment issues can aid in managing ongoing headaches and supporting recovery.
Finding the Right Diagnosis for Headaches Linked to Concussions and Neck Injuries
An accurate diagnosis is essential to understand the nature of your headaches and determine whether they stem from overlooked brain injuries. A physician may use several diagnostic tools in the process, including the following:
- Medical history review: Helps understand headache onset, previous injuries, and pre-existing conditions that may impact the cervical spine, such as degenerative disc disease and spinal stenosis.
- Physical examination: Assesses neurological functions and neck mobility.
- Neurological assessments: Help evaluate brain function and identify potential damages.
- Imaging tests: Techniques like MRI, X-rays, and CT scans may be used to create detailed views of head and neck structures.
- Cervical spine evaluation: Checks for upper neck facet joint injury or instability in the spine, which may impact the stability of the head and, in turn, surrounding muscles and tissues.
One of the key things to help diagnose upper neck injury is looking for injuries to the ligaments that hold the head to the neck. DMX technology, can capture real-time neck movements and reveal hard-to-diagnose instabilities.
DMX Technology
Digital motion X-ray technology is a dynamic imaging technique that may aid in diagnosing neck injuries. Unlike traditional X-rays that capture still images, DMX provides a real-time view of the cervical spine in motion.
This dynamic approach reveals issues that remain hidden in static images, such as abnormal vertebral movements or ligament laxity. The X-ray records these movements and collects data, highlighting any instability or misalignment, especially in key but hard-to-diagnose structures like the alar or transverse ligaments.
This technique’s advantage is rooted in its ability to replicate daily stresses on the neck in a controlled setting, offering unparalleled insights into the mechanical function and health of the cervical spine.
Work with CSC on a Treatment Plan That Addresses the Right Condition
Recurring headaches after a concussion or pain in the neck or at the base of the skull may indicate ongoing issues that need prompt medical attention. At the Centeno-Schultz Clinic, our physicians utilize a comprehensive, whole-person approach to headaches. Using advanced diagnostic tools, like DMX technology, we seek to better understand the causes behind cranio-cervical instability, neck injury symptoms, and persistent headaches.
If your upper neck joints are injured, our physicians are specialists in injecting substances like PRP, which show great promise in helping damaged joints heal. These are highly specialized injections that require advanced fluoroscopy using digital subtraction angiography and are only performed by a handful of experienced physicians in the U.S.
If the upper neck nerves have been injured, our physicians can inject growth factors derived from the patient’s platelets to help heal those injured nerves. This is an ultrasound-guided injection that targets specific nerves that have been damaged.
Our clinic also offers percutaneous injection of the craniocervical ligaments (PICL), an interventional orthobiologic procedure designed to support upper cervical spine stability. This approach aims to enhance neck function and may help alleviate discomfort associated with craniocervical instability.
Unlock the right condition causing your symptoms with DMX technology at the Centeno-Schultz Clinic, offering precise diagnostics and personalized treatment options.