Post-Concussion Syndrome (Persistent Concussion Symptoms)

Post-concussion syndrome (PCS), or persistent concussion symptoms, occurs when concussion symptoms last longer than a few weeks. These symptoms can include trouble thinking, mood changes, and physical issues like headaches. The causes often link back to the initial head injury, but underlying neck issues, like craniocervical instability, can worsen PCS. It’s also possible that upper neck issues can remain, after the concussion has healed and can mimic concussion symptoms.
Symptom type, intensity, and duration can vary, meaning that each person might need a different approach to their treatment.
The Centeno-Schultz Clinic uses advanced tools like digital motion X-ray (DMX) to find and address neck problems that may worsen or mimic PCS. Through comprehensive, personalized approaches to treatment, the physicians at the Centeno-Schultz Clinic aim to relieve symptoms while supporting long-term neck and spine health.
What Is Post-Concussion Syndrome?
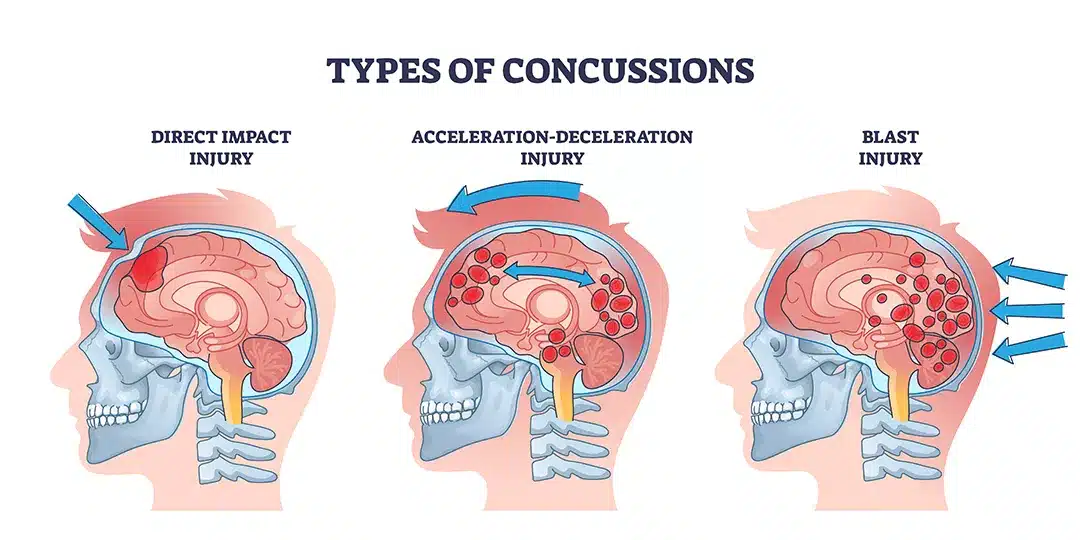
PCS is a condition where the symptoms of a concussion extend beyond the typical recovery timeframe. A concussion occurs when the head experiences a jolt or blow. This injury can trigger several reactions, including:
- Axonal shearing refers to damage to the axon or brain tissues, which can disrupt neural communication.
- Inflammation: This leads to swelling and increased sensitivity in the brain, which cause pain and headaches.
- Neurotransmitter imbalance: Brain injury can cause an increased release of chemicals, like neurotransmitters, and alter neural communication, which can affect brain function.
Research shows that around 90% of concussion symptoms are temporary, resolving within 10-14 days as the injured tissues begin to heal. However, sometimes, these symptoms last longer, for months or years. This is known as post-concussion syndrome, and it can occur due to improper healing or complications affecting the brain or neck.
Clinically, PCS is diagnosed when concussion patients continue to experience three or more of the following symptoms:
- Headache
- Dizziness
- Fatigue
- Irritability
- Insomnia
- Difficulty with concentration or memory
A 2019 study suggests that 10-15% of people experiencing a concussion develop PCS, while 2018 research found that this percentage may be as high as 41.5%.
PCS can significantly impact daily life by causing headaches, dizziness, cognitive impairments, and emotional disturbances.
How To Identify Persistent Concussion Symptoms
PCS can arise because the brain struggles to return to normal after injury. This can be due to risk factors like the type and severity of head trauma but also due to underlying neck issues.
If left untreated, PCS can significantly impact all aspects of life well after the initial concussion. Beyond pain, symptoms like cognitive difficulties, emotional disturbances, and physical complaints can be debilitating, affecting both work and personal interactions. Recognizing these symptoms is crucial for getting appropriate care and addressing potential long-term effects.
Cognitive Difficulties
Cognitive difficulties manifest when the brain, impacted by a concussion, struggles to process information as efficiently as it did before the injury. This condition can arise due to physical tissue damage, like axonal shearing, inflammation, swelling, or chemical imbalance in the brain. However, remember that symptoms like “brain fog” are also common in patients who have injured their upper neck. Hence, cognitive difficulties can be due to the original concussion, the upper neck, or both.
Common cognitive difficulties include:
- Difficulty remembering: Axonal shearing can damage memory storage and retrieval pathways. This can lead to memory gaps or delays in recalling information.
- Problems with focus and attention: Swelling and chemical imbalances alter neural activity, making it difficult to maintain concentration.
- Mental fog: Inflammation and disrupted communication between neurons slow down cognitive processing, creating a sensation of fatigue and clouded thinking. This is also called “brain fog”.
- Impaired problem-solving skills: Tissue damage and neurotransmitter disruption impact the brain’s ability to formulate and execute plans. This can affect both work tasks and leisure time.
Emotional Disturbances
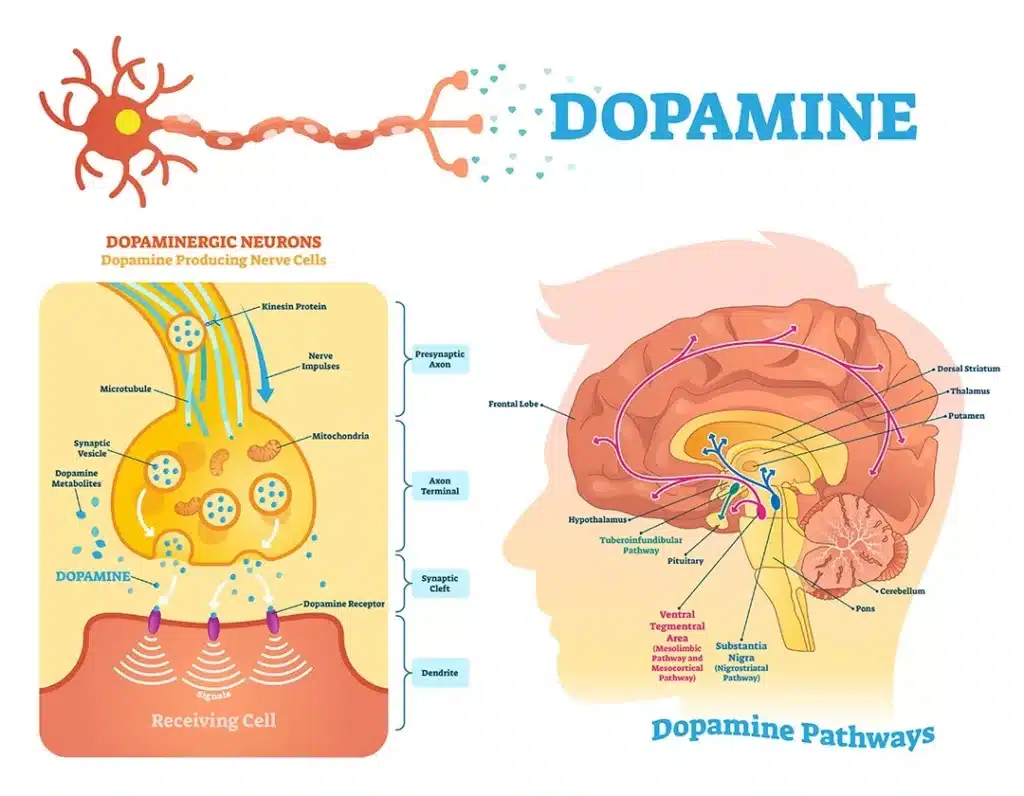
PCS can alter the brain’s chemistry, triggering an excessive release of chemicals like neurotransmitters.
Neurotransmitters are chemical messengers that facilitate communication between neurons, and they can impact mood and emotions. For instance, serotonin regulates mood and is often dubbed the “feel-good” neurotransmitter. Imbalances in these chemicals are linked to issues like depression and anxiety.
Similarly, dopamine plays a role in reward and pleasure. When its production is disrupted, it can lead to feelings of apathy or decreased motivation. These neurotransmitter shifts in PCS contribute to emotional disturbances, deeply affecting relationships, self-esteem, and happiness.
Common emotional symptoms include:
- Feelings of nervousness: When the brain’s stress response is overly active, it can lead to constant anxiety. Feeling chronically anxious can disrupt concentration and sleep patterns, creating a cycle of increased stress.
- Increased frustration or mood swings: Imbalances in neurotransmitters can disrupt mood and emotional stability. This may result in unexpected emotional outbursts or sudden mood changes, interfering with social interactions and relationships.
- Lack of energy or drive: Ongoing fatigue and stress can reduce motivation and energy levels. This feeling of being constantly tired can make daily tasks seem daunting and contribute to a sense of hopelessness.
Also realize that chronic neck pain, which is common in PCS patients, can also cause emotional issues that can mimic those found in PCS.
Sensory Impairments
Damage to the brain’s tissues can impair how sensory and motor signals are processed. This can alter how the brain interprets environmental signals, impacting daily life functions such as driving or working in certain conditions. Common symptoms include:
- Vision disturbances: Injuries to brain parts that control vision can lead to symptoms like blurred vision or light sensitivity. These problems can inhibit focus, increase the risk of injuries, and make tasks like reading or studying difficult.
- Motion-related nausea: When the brain struggles to handle sensory signals, patients can experience dizziness and nausea, especially when moving. This condition can make simple activities challenging, such as getting out of bed or riding in a car.
Again, it should be noted that the upper neck can also cause both of these issues. In that case, the position sense data constantly fed to your inner ear and visual systems by the upper neck is disrupted, which can cause visual disturbances and nausea.
Physical Complaints
The neurobiological changes that occur after a concussion can also lead to physical symptoms. These stem from brain inflammation and swelling, as well as disrupted neural pathways and improper nerve signal processing. Over time, these symptoms can limit physical capabilities and reduce quality of life. Common signs include:
- The sensation of pressure in the head: Headaches and sensations of pressure often result from inflammation, which is part of the body’s response to injury. The inflammatory response increases the blood flow to the injured tissues to support healing, but it can cause swelling, bruising, and a sensation of pressure. Pressure in the head can cause headaches, disrupt focus, prevent relaxation, and reduce sleep quality.
- Neck pain: Neck pain, or cervicalgia, can stem from injuries that occur alongside a concussion. For example, in a whiplash injury, the neck muscles or ligaments become strained or overstretched. The facet joints in the neck, can also get injured. Additionally, muscle tension can occur after trauma as the body attempts to support injured tissues, increasing stiffness and pain.
- Chronic fatigue: After a concussion, the body uses extra energy to support healing, leading to chronic fatigue. A 2021 study found that many people experience severe fatigue for years post-trauma, with 73% still affected after five years. This fatigue makes daily tasks feel overwhelming and impacts work and social life, despite sleep or rest.
- Balance issues: Concussions disrupt the vestibular system, which helps maintain balance. This can affect how the body perceives itself in the surrounding space (proprioception) and lead to difficulties with coordination and balance. Balance issues can increase the risk of falls and make walking on uneven surfaces more challenging. Remember, your upper neck can also cause poor balance, dizziness, or vertigo.
Brain Fog
Brain fog is one of the hallmark symptoms of Craniocervical instability. It is characterized by slow thinking, difficulty focusing, confusion, lack of concentration, forgetfulness, or haziness in thought. The severity of symptoms varies from patient to patient. Ever had a bad hangover or high fever and had trouble concentrating or completing simple tasks? This brain fog. Some patients describe it as a generalized haziness in thought as if cotton were stuck in the head. In addition to cognitive impairments, many patients also report generalized mental fatigue making complex tasks almost impossible. The exact cause of brain fog is unknown. Possible explanations include…
Read More About Brain FogChronic Fatigue
Have you ever had a challenging all-day hike, athletic endeavor, or worked a double shift and felt exhausted the next day? Later that day or the next morning, moving across the room may have seemed almost impossible and took herculean power. Now image this occurs on a daily basis without any provocation. 24/7 simple tasks are nearly impossible due to a lack of strength and energy. This is chronic fatigue, and it is one of the common symptoms associated with craniocervical instability. Severity can vary and in severe cases, patients are confined to their beds. Aggravating and alleviating factors often times can not be identified.
Read More About Chronic FatigueChronic Headaches
Do you suffer from chronic headaches? Maybe it’s a daily issue, maybe once a week, maybe even less often, but one thing’s for sure—when a chronic headache kicks in, it can be a real pain in the neck, literally. In order to effectively address chronic headaches, you have to first determine if the pain is caused by a problem in your neck. Let’s take a look at a few neck issues that can cause headaches: Weak neck muscles – The head, on average, weighs about ten pounds, so when the neck muscles are weak, it can make your head feel a bit like a bowling ball that your neck can’t quite balance. There are many muscles that, along with the cervical spine, work together to help support the neck and aid movement…
Read More About Chronic HeadachesTinnitus
Remember the ringing in your ears after a loud rock concert or highly charged sporting event? It is that ringing or buzzing sound that slowly improves the next day over several hours. Unfortunately for some individuals, the ringing in the ears is not due to an external event. Even worse is it does not resolve over time. This condition is called tinnitus. It is a medical condition characterized by ringing or other noises in one or both ears NOT caused by an external sound. Other individuals cannot hear the ringing that patients describe. It is a common problem. It affects approximately 15-20% of individuals.
Read More About TinnitusMethods for Evaluating and Diagnosing Symptoms
Evaluating PCS isn’t always straightforward. According to a 2022 study, PCS is often misdiagnosed, as its symptoms overlap with the ones of conditions like depression, attention deficit disorders, or sleep disorders.
A comprehensive and structured approach is essential to determine the causes and nature of persistent concussion symptoms. A thorough diagnostic process also looks at underlying conditions, like upper neck injury or instability, that may contribute to symptoms and increase the risk of complications.
Typical diagnostic methods include:
- Patient history and medical background: A detailed history helps identify prior concussions or head injuries and pre-existing conditions, such as neck issues. This helps determine factors contributing to persistent symptoms, such as untreated prior injuries.
- Physical examination: A physician may conduct several tests, including assessments of balance, coordination, and sensory responses, to detect issues pointing to PCS, such as dizziness or reduced motor function. In addition, a thorough neck examination, which involves pressing on each of the upper neck facet joints, neck range of motion, and other tests, is critical.
- Imaging tests: CT scans and MRIs are primarily used to rule out acute brain injury, which can mimic PCS and serious head injury complications like bleeding. They also play a crucial role in evaluating possible structural anomalies contributing to PCS symptoms. In addition, neck imaging is a key part of this diagnostic work-up. For example, ruling out craniocervical instability or CCI may requirement movement-based imaging like DMX.
- Laboratory tests: Lab tests can rule out other conditions with overlapping symptoms, such as metabolic issues, arthritis, or infections. They can also help diagnose co-existing conditions that may be aggravating PCS.
- Neurological evaluations: These are used to evaluate cognitive, sensory, and motor functions. Tools like the Glasgow Coma Scale or neuropsychological tests can determine impairments caused by brain trauma.
Causes and Risk Factors of Post-Concussion Syndrome
PCS often follows a concussion, and it’s more likely if:
- You experienced previous head injuries
- Your concussion symptoms were severe
- You reported additional injuries, like a skull fracture
- You experienced concussion complications
However, risk factors don’t just relate to the type and severity of head trauma. They include the following.
Head Injury
The type of head trauma you experience can impact the risk of PCS. In particular, you may be more at risk of persistent concussion symptoms after:
- Skull fracture: A traumatic head injury that causes a break in the skull is considered extremely severe. It can lead to intense symptoms—such as pain and swelling—and is often associated with additional complications like brain contusions or bleeding. These injuries extend recovery and cause major brain function disruptions, increasing the risk of PCS.
- Midline shift: Occurs when swelling or bleeding pushes the brain out of its normal central alignment. This shift can interfere with the brain’s functions by placing undue pressure on certain parts of the brain and causing sustained injury. These complications can make recovery more challenging and can intensify the symptoms of PCS.
ADHD
ADHD, or attention-deficit/hyperactivity disorder, is a condition that affects how the brain manages attention, controls impulses, and regulates hyperactivity. In patients with ADHD, neurotransmitter imbalances are common. Symptoms like reduced focus and attention occur because of altered chemicals in the brain.
These mechanisms can also make the brain more prone to disruptions like PCS:
- Attention challenges: People with ADHD naturally struggle with focus because of alterations in neural pathways. A concussion can disrupt these pathways further, making concentration even harder.
- Behavioral issues: ADHD can lead to impulsivity and hyperactivity. When coupled with a concussion, managing behaviors can become more difficult as the brain struggles to regulate emotions and cognitive functions.
- Increased anxiety: Increased anxiety is common in individuals with ADHD. A head injury can increase stress signals in the brain, aggravating nervousness, anxiety, and irritability.
- Slower recovery: The neurochemical imbalances in ADHD can also affect how the brain’s healing mechanisms function. This can slow the recovery process and make PCS symptoms last longer.
Hypermobile Ehlers-Danlos Syndrome
Hypermobile Ehlers-Danlos syndrome is a disorder that affects connective tissues, impacting joint flexibility and stability.
Those with this condition face increased risks of joint and tissue injury when experiencing physical trauma. For example, in the event of a concussion caused by a whiplash, individuals with hypermobile Ehlers-Danlos syndrome are more prone to additional issues, like neck and spine injury.
When these problems occur alongside a concussion, they can increase the risk of persistent concussion symptoms, including headaches, pain, muscle tension, and neck instability. Combined, these issues can prolong PCS symptoms and delay recovery.
Craniocervical Instability
Craniocervical instability occurs when there is an abnormal and excessive movement at the joints where the skull meets the spine and elsewhere in the upper neck. This abnormal motion results in ligament injury and stretching. This instability can aggravate the symptoms of PCS by increasing strain on key areas, like the neck and brain stem, during or after a concussion.
Individuals with this condition are more likely to experience prolonged or severe PCS symptoms, including dizziness and headaches. Misdiagnosing or overlooking the mechanical stress that craniocervical instability can cause can lead to long-term head and neck issues.
In addition, craniocervical injuries without instability are also common. These can involve injuries to the upper neck joints, nerves, or other structures and can mimic PCS.
Conventional Treatment Options
Conventional treatments for PCS focus on managing symptoms and supporting the brain’s healing process. Common strategies include:
- Rest and activity modification: This approach helps create an optimal healing environment for the brain and prevent further injury. As symptoms ease down, physicians may recommend the gradual reintroduction to activities to avoid setbacks.
- Medication management: Medications are used to manage specific symptoms of PCS but don’t treat underlying issues. For example, nonsteroidal anti-inflammatory drugs like ibuprofen can be used for headaches, and ondansetron for nausea. However, long-term use of these medications can lead to side effects, including an increased risk of heart attack, stroke, and kidney dysfunction.
- Physical therapy: This involves physician-guided exercises that help improve balance and muscle strength, while easing muscle tension and improving posture. Combined, these actions can alleviate headaches and neck pain.
- Cognitive rehabilitation: This treatment uses mental exercises and techniques to help restore memory and attention. It focuses on rebuilding cognitive skills through tasks that improve focus and problem-solving abilities, assisting individuals to manage daily and work tasks.
- Neurological rehabilitation: This focuses on restoring sensory functions affected by PCS through targeted therapies. For example, vestibular therapy addresses balance issues by retraining the brain’s coordination systems, while vision therapy improves visual processing, which helps with light sensitivity or blurred vision.
- Psychological support: PCS can cause emotional issues like mood swings and irritability. It can also have a profound impact on mental health and daily life. In a 2024 study conducted on 208 people, 46% of patients with PCS also had depression symptoms. Therapies like cognitive behavioral therapy (CBT), counseling, and mindfulness meditation, can help provide support through the psychological symptoms of PCS.
Why Some Treatments Fail And Persistent Concussion Symptoms Continue
As mentioned above, the experience of PCS is unique for each patient. For some, the symptoms are mild and temporary, while in other cases, the pain, impaired cognitive function, and emotional imbalances can be debilitating.
Additionally, not everyone responds in the same way to treatment. Understanding why some treatments fail and symptoms continue is essential in managing PCS. Common reasons include:
Variability in Healing and Response to Treatment
While concussion symptoms often improve within 10-14 days, the effects of PCS can last months or years. Patients’ healing times vary significantly, influenced by factors like age, health, and the severity of the initial concussion.
Additionally, research indicates that PCS symptoms can become permanent if not properly addressed. A study on 110 PCS patients found that only 27% eventually recovered, and 67% of these recovered within the first year. Among the factors that reduced the chances of recovery are non-compliance with medical advice and experiencing multiple symptoms.
The same study suggests that, while symptoms can vary from one person to another, symptom patterns are predictable. If not treated within three years, they are likely to become permanent.
Treating Symptoms Instead of the Underlying Condition
Many conventional treatments focus primarily on managing symptoms rather than addressing the root causes of PCS. This approach results in temporary relief at best, while it leaves underlying issues unaddressed.
For instance, medications might alleviate headaches or dizziness but do not solve neurological or vestibular dysfunctions that are at the root of ongoing symptoms.
This focus on symptoms rather than on underlying causes can lead to a cycle of recurring pain, dissatisfaction with treatment results, and risk of medication side effects.
Undiagnosed Neck Injuries
As noted above, the root causes of persistent concussion symptoms are often misdiagnosed.
As the saying says, the head bone is connected to the neck bone. Conditions like whiplash or upper cervical spine dysfunction can mimic or worsen PCS symptoms such as headaches, dizziness, and cognitive disturbances. These upper neck-related issues are often overlooked, possibly due to inadequate diagnostic processes or a focus on brain injury.
Because of this, it is important to seek expert diagnosis and treatment. Specialized healthcare providers, such as the Centeno-Schultz Clinic, understand the impact of underlying upper neck issues. Using advanced diagnostic techniques, specialists can assess the spine and head as one integrated structure, examining it in motion and taking into account all the factors that may be contributing to your symptoms.
Centeno-Schultz Clinic’s Expertise in Diagnosing Upper Neck Injuries
Certain underlying issues, including neck injuries and musculoskeletal disorders, can contribute to prolonged concussion symptoms. These injuries, such as craniocervical instability, are often overlooked in conventional assessments. When left untreated, they can worsen symptoms and lead to complications in the future.
At the Centeno-Schultz Clinic, our physicians specialize in using advanced diagnostic technologies, such as the digital motion X-ray. As part of our comprehensive approach, we assess the spine as an integrated structure, taking into account a range of often overlooked factors that may contribute to pain and dysfunction.
DMX or Upright Movement MRI Technology for Accurate Detection of Upper Cervical Issues
Digital motion X-ray is an innovative imaging technique that captures dynamic images of the cervical spine. These dynamic assessments help in determining conditions that would otherwise be difficult to diagnose, such as craniocervical instability. Craniocervical instability occurs when ligaments in the neck become lax, causing excessive movement between the skull and spine. Unaddressed, this can complicate other conditions, like PCS, and lead to pain and neurological symptoms over time.
Unlike static imaging methods like routine MRIs, DMX allows physicians to visualize the neck in motion. This is critical for diagnosing instabilities caused by injured or lax ligaments and determining how structures in the cervical spine are affected during movement. Recent findings show that DMX is a highly effective technique, with a 95% accuracy rate for detecting neck injuries like craniocervical instability.
Upright MRI with movement is another technology we use at CSC to diagnose upper neck issues. This technology can see soft tissues like a routine MRI, but instead of lying face up in a tube, the patient is seated, mimicking normal weight bearing, and asked to move the neck.
At the Centeno-Schultz Clinic, the use of DMX and upright MRI provides our physicians with important insights that can guide treatment. Thanks to a comprehensive view of the cervical spine and its components, treatment plans can be tailored to address not just symptoms but also underlying musculoskeletal conditions.
Detect the Root Issue Behind PCS and Get the Right Treatment
If you have been experiencing ongoing symptoms affecting the head and neck, getting an accurate diagnosis and a tailored treatment plan is paramount to prevent complications and restore function.
At the Centeno-Schultz Clinic, we understand how frustrating it can be to suffer from ongoing symptoms and see several treatments fail. That is why we employ advanced techniques, like DMX imaging, to provide you with the clarity you deserve. Consult with our physicians today to find out whether this is the right option for you.
Get Your Post Concussion Syndrom Checked by a Professional
If you have been dealing with a Post Concussion Syndrome and are contemplating surgery, call and set up an evaluation with one of our experts who can further evaluate you and your candidacy for a surgery avoidance.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreOther Resources for Post Concussion Syndrome
-
Exploring the Long-Term Effects of Post-Concussion Syndrome
Post-concussion syndrome (PCS) (aka persistent post-concussion symptoms) is a condition that often arises after a concussion, which is one type of traumatic brain injury (TBI). It is characterized by symptoms that persist long after the initial injury, leading to significant long-term effects that can impact both physical and mental health. While most people recover from…
-
Concussion Headaches And Why the Right Diagnosis Is Critical
Concussion headaches often occur after traumatic brain injuries. They can result from mechanical impacts and chemical changes in the brain. These headaches can cause persistent pain, sensitivity to light, and cognitive issues. It is important to accurately diagnose them to distinguish them from other types, like migraines or tension-type headaches. If untreated, they may lead…
Struggling with post-concussion symptoms and ineffective treatments? A precise diagnosis is key. Contact us today for expert evaluation and personalized care.