Thoracic Spine Tumor: Symptoms, Causes, and Treatment Options

Back pain is one of the most common health problems worldwide, affecting a staggering 620 million people each year. But this symptom is often non-specific, meaning that it can indicate a range of conditions.
For some, it’s nothing more than a temporary annoyance caused by a minor injury or incorrect posture, which goes away with some rest and activity modifications. For others, however, back pain can be an acute or chronic problem stemming from severe underlying conditions, such as thoracic spine tumors.
Thoracic spine tumors grow on the middle segment of the spine, causing a mix of symptoms – some subtle, others severe – and progressing into becoming a medical emergency and significantly impacting the person’s well-being. Fortunately, thanks to today’s advances in regenerative medicine, patients can look beyond pharmaceutical and invasive procedures to improve their quality of life. Discover how in this guide by the Centeno-Schultz Clinic.
Anatomy of the Thoracic Spine
The spine is subdivided into different regions:
- The cervical spine: neck area
- The thoracic spine: the middle of the spine, running from the upper-back to mid-back
- The lumbar spine: lower back
- Sacrum: the bottom of the spine
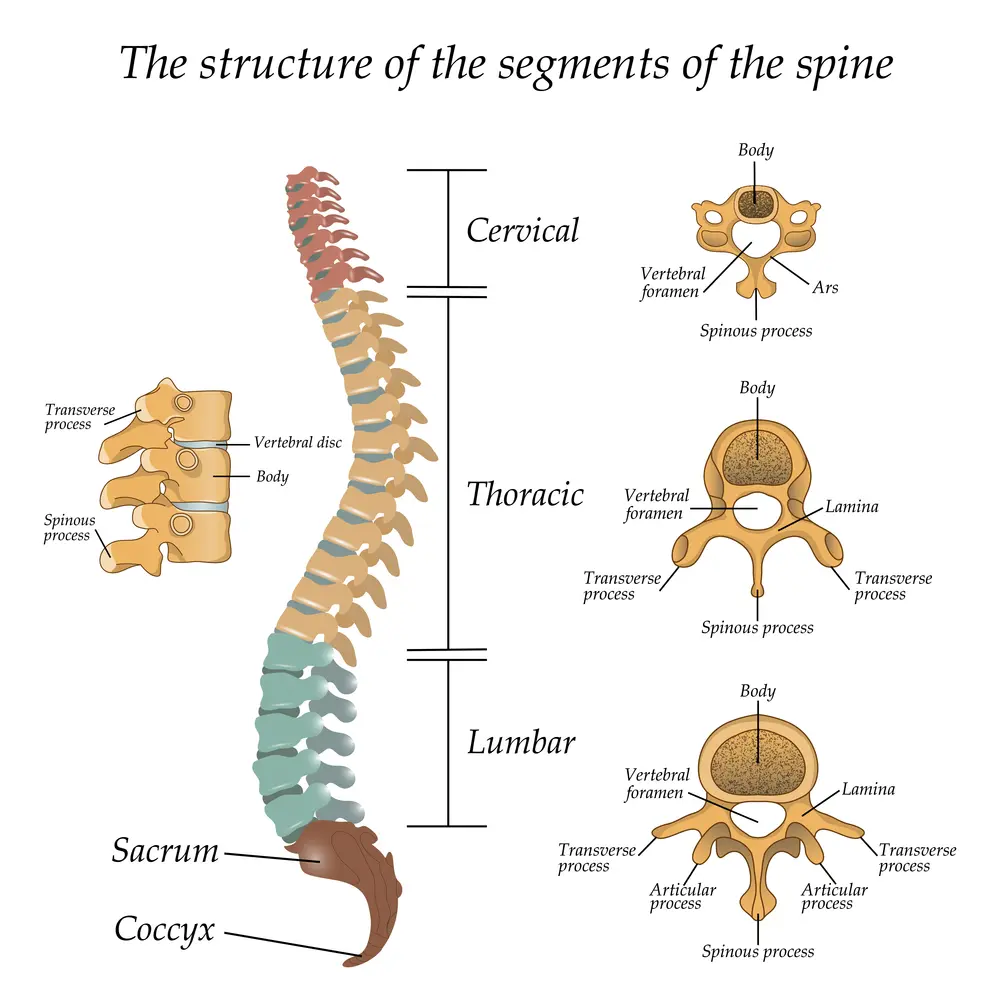
The thoracic spine consists of 12 vertebrae, each cushioned by intervertebral discs, which absorb shock and friction from movement and maintain spine flexibility. This spine segment stretches from the base of the neck to the abdomen, and it serves as a vital support structure that protects the spinal cord while allowing the upper body to move and flex.
From the thoracic spine stem are 12 nerve pairs exiting the two sides of the vertebrae. These nerves innervate the muscles and skin of the thorax and abdomen. They are responsible for controlling intercostal muscles, aiding in respiration, and providing sensory input to parts of the skin. They also contribute to the function of some abdominal organs.
What Are Thoracic Spine Tumors?
Tumors are abnormal growths of cells that can develop in various parts of the body. They occur when cells divide uncontrollably, forming lumps or invading surrounding tissues. A spinal tumor is a growth that occurs within or near the spinal cord or spine.
Spine tumors can occur anywhere along the spine, but they most commonly affect the thoracic and lumbar regions. They can develop in various tissues and locations in and around the spine, including:
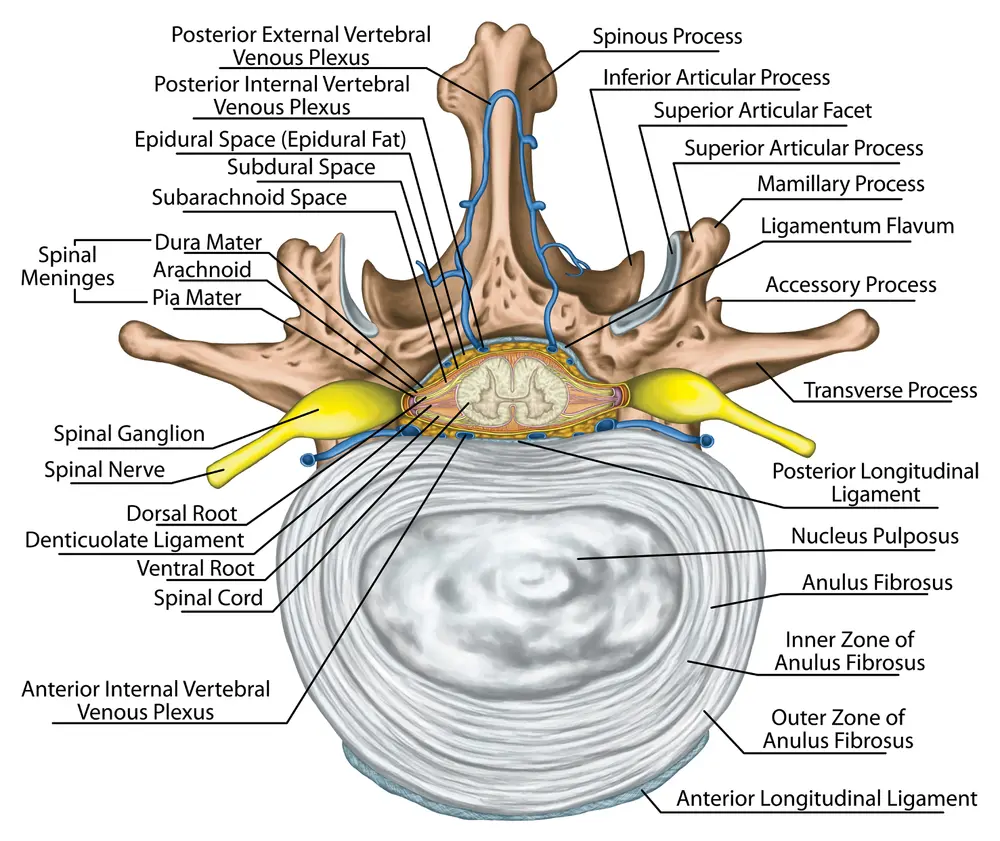
- Bones of the spine, i.e.: vertebrae, and the bone marrow inside them
- The cartilage between the vertebrae, which protects the spinal joints
- Spinal discs, which cushion the vertebrae
- The blood vessels responsible for delivering nutrients and oxygens to the components of the spine
- Peripheral nerves and nerve roots, as they exit the spine and begin to innervate areas of the body
- The membranes that enclose the spinal cord, which include the dura mater, pia mater, and arachnoid mater
- The spinal cord
Depending on where the tumor is located, it may be classified as:
- Extradural tumor: this type of tumor is located outside the dura mater, which is the thin covering around the spinal cord. Although these tumors may involve the vertebrae, they don’t usually affect the spinal cord. Spine tumors account for 15% of central nervous system tumor cases, and around 55% of them develop in this area.
- Intradural tumor: This type of tumor develops inside the dura membrane and may or may not involve the spinal column. Intradural tumors are further classified into:
- Intramedullary tumors: Grow inside the spinal cord and account for around 5% of spinal tumors.
- Intradural-extramedullary tumors: Grow inside the dura but outside the spinal cord and account for around 40% of spinal tumors.
These tumors can also be categorized into primary and secondary tumors:
- Primary tumors originate within the spine, are generally less common, and are mostly found in intradural tumor cases. They also tend to be benign (noncancerous).
- Secondary or metastatic tumors are far more common and are usually malignant (cancerous). They spread from tumors in other parts of the body and they tend to be contributors to extradural tumor cases (which, as we’ve seen above, make up for the greatest percentage of spine tumor cases).
In-depth: tumor vs cancer – what you need to know
When dealing with tumors, it is important to understand the difference between various types of abnormal growths and their implications:
Benign tumor: These are non-cancerous growths that do not spread, but they are not harmless. They can still cause pain or neurological issues.Malignant tumor: These are cancerous growths that grow faster and can invade nearby tissues or spread to other parts of the body.Tumor-like masses: Include cysts and other non-neoplastic lesions that may mimic tumor symptoms but differ in nature and may require a different treatment.
Although anyone can be affected by a spinal tumor, they are more likely to develop in people who have certain genetic conditions or other types of cancer – especially if these cancers affect areas around the thoracic spine, such as lung, breast, and prostate cancers.
Below, we’ll look at the different types of spine cancer in more detail.
Primary Tumors
Primary tumors originate from cells within the thoracic spine itself. They can be benign or malignant, categorized based on the specific cell types they develop from. However, the majority of primary spine cancers are benign: only 20% of primary spine tumor cases are malignant, accounting for less than 0.05% of all newly diagnosed tumors.
Depending on their cell of origin, there can be different types of primary tumors developing in the spine, including:
- Osteogenic tumors. These are tumors that develop from bone cells and include aggressive and malignant types, like osteosarcomas.
- Neurogenic tumors. Arising from nerve cells, they include schwannomas and neurofibromas that may compress spinal nerves.
- Meningiomas. Usually benign, these tumors stem from the meninges (the protective layers) covering the spinal cord.
- Chordomas. These are rare and slow-growing tumors, and they originate from notochordal remnants (leftover tissues from the embryonic notochord, which serves as the “scaffolding” for the adult spine).
- Hemangiomas. These are benign vascular tumors, which are mostly asymptomatic. However, if they develop further, they can cause pain and the collapse of vertebrae in rare cases.
So far, research hasn’t been able to pinpoint the exact cause of primary spinal tumors. However, they are more common in adults aged 65-74 and in children aged 10-16. Possible risk factors include:
- Exposure to cancer-causing chemicals
- Weakened immune systems (which can cause spinal cord lymphomas, or cancers that affect a type of immune cells)
- Certain genetic components
Secondary (Metastatic) Tumors
Secondary (metastatic) spinal tumors originate from cancers elsewhere in the body that metastasize (or spread) to the spine. This often occurs when cancerous cells from other areas of the body travel through the bloodstream or lymphatic system from the primary tumor. The spine, which has a significant blood supply and is located close to lymphatic and venous systems, is particularly at risk.
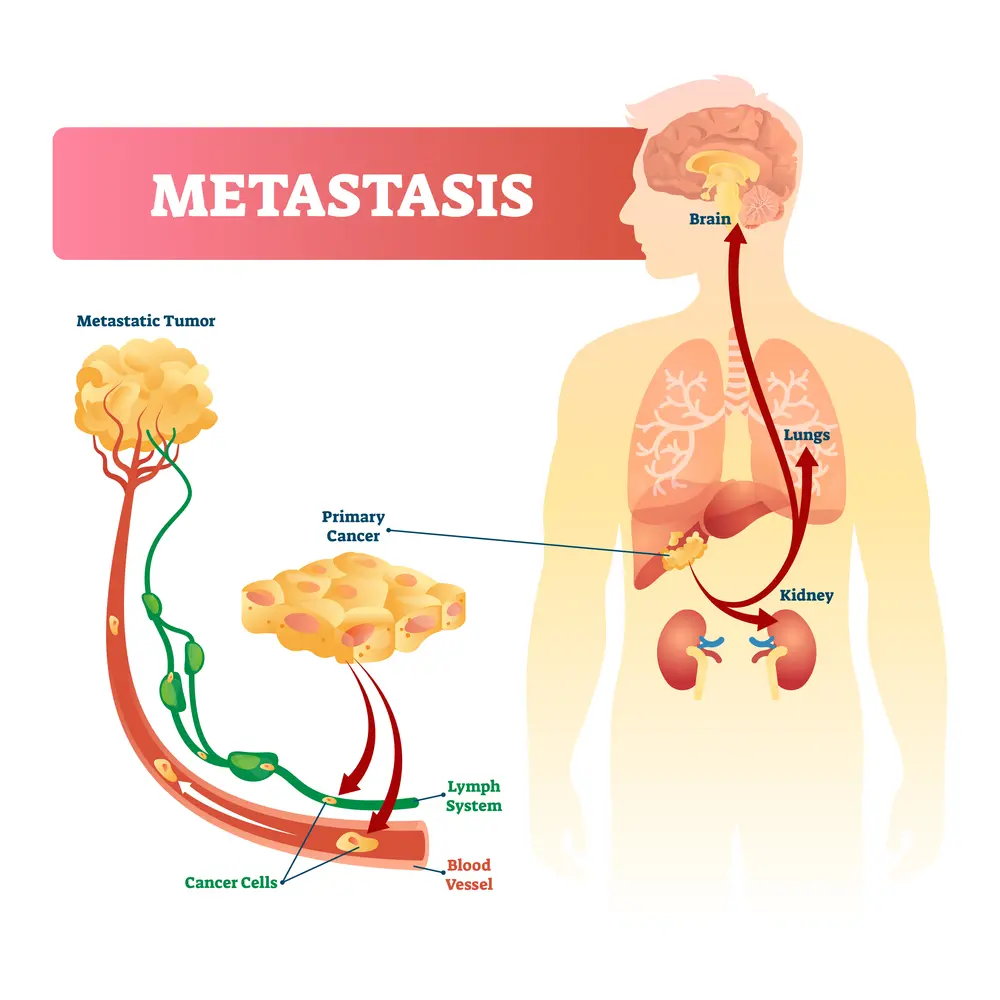
It is estimated that metastatic spinal tumors account for 97% of spinal tumors. Up to 70% of patients with systemic cancer are likely to develop spinal metastasis, and the thoracic section of the spine is most frequently affected, accounting for 60-80% of cases.
The most likely cancers to metastasize to the spine include:
- Breast cancer. Breast cancer metastases account for 21% of spinal tumors. They tend to spread to bones, including the thoracic spine, leading to pain and fractures.
- Lung cancer. Frequently metastasizes to the spine, accounting for 14% of spine cancer cases, and often causing significant neurological symptoms.
- Prostate cancer. Prostate cancer metastases account for 8% of spine tumor cases. They tend to spread to bones, affecting the vertebrae and other spinal components.
- Renal cell carcinoma. This cancer affecting kidney cells is responsible for 5% of spine tumor cases.
- Thyroid cancer. Can metastasize to the spine due to its location, though less frequently. It may cause local pain and structural instability.
Given the fact that most tumors that are able to spread are malignant, most secondary tumors in the spine are also cancerous, and they often indicate advanced stages of the disease.
Symptoms of Thoracic Spine Tumors
Both primary and metastatic thoracic spine tumors often begin without obvious symptoms, or with non-specific symptoms, like back pain. Because of this, diagnoses are often delayed, allowing the tumors to progress undetected until the symptoms become severe or debilitating.
The type and intensity of symptoms of spinal tumors depend on several factors, including:
- The nature and type of the tumor
- The size of the tumor
- Where the tumor is located in the spinal column
As the tumor grows, symptoms tend to worsen. Recognizing this progression early on helps seek an adequate diagnosis and begin treatment as soon as possible.
Pain
Pain is the most common symptom associated with spinal tumors. Research shows that, in up to 16% of patients, the clinical manifestation of spinal tumors occurs with spinal cord compression symptoms, such as pain. This happens when abnormal tissue growths exert pressure on nearby structures, including nerves, bones, blood vessels, and the spinal cord itself. Additionally, as the tumor grows, it can cause inflammation, which further exacerbates swelling and pain.
Pain in thoracic spine tumor cases can take on many forms, including:
- Radiating pain to the chest, abdomen, or arms. Tumors impinging on nerve roots that innervate the chest, abdomen, arms, and extremities can prevent nerve signals from correctly traveling to and from the brain. This translates into nerve pain, such as burning sensations, “pins and needles”, and numbness. This is known as radicular pain, and it often feels sharp and shooting.
- Back pain. Back pain can occur when the tumor compromises the stability of the spine structure, leading to problems such as bulging discs and fractures.
- Pain in the thoracic spine. Localized tumor growth or compression directly impacts the thoracic spine area, inducing sharp or constant pain.
Although back pain tends to be a non-specific symptom, there are telltale signs that it may indicate a tumor as opposed to other conditions, like sprains and strains. These signs include:
- It is not associated with an injury or stress but gets worse with exercise, coughing, or sneezing.
- It causes deep, aching sensations that start slowly and increase over time.
- It can occur at night and even disrupt sleep.
- It doesn’t respond to pain medications.
Neurological Symptoms
Thoracic spine tumors can lead to neurological symptoms when the abnormal growths press on the spinal cord or the spinal nerves, disrupting the normal signaling pathways.
Depending on what nerve fibers are affected and the stage of the tumor, these symptoms may appear as mild numbness and tingling in the hands but can develop into debilitating pain, weakness, and disability across the body.
Neurological symptoms of thoracic spine tumors include:
- Weakness or numbness in extremities. Tumors can compress nerve roots or the spinal cord itself, leading to a loss of function or sensation. Sufferers may also experience difficulties with fine motor skills, which involve the use of small muscles in the hands, such as writing or drawing.
- Difficulty with balance and coordination. Myelopathy (spinal cord compression by the abnormal growths) can prevent the normal transmission of motor signals, which can lead to problems with proprioception, sitting, standing, walking, and maintaining balance.
- Radicular pain (radiating pain along nerves). Nerve root irritation or radiculopathy (pinching of the nerve roots) interferes with signal transmission along the affected nerve’s path, causing pain in several other areas of the body, from hands and arms to the legs.
Other neurological symptoms include:
- Bowel and bladder issues
- Tingling
- Numbness
- Muscle weakness, loss of grip strength
- Involuntary muscle movements, like cramps and fasciculations
- Paralysis
Other Signs and Symptoms
Thoracic spine tumors – like other cancers – may cause systemic symptoms that spread beyond the local spine area. These tumors might affect metabolic processes, immune system responses, or other body functions depending on their size, aggressiveness, and nature (e.g.: the type of cells they generate from). Some of these systemic symptoms include:
- Fatigue: The body’s energy is used to combat the tumor and maintain normal function, which can cause you to feel unusually tired, unable to concentrate, and fatigued.
- Unexplained weight loss: Tumors can alter metabolism or secrete substances that increase metabolic rate, leading to unexpected weight loss.
- Fever or night sweats: These are common systemic responses to malignancy, often indicating that your body’s immune system is attempting to respond to the tumor.
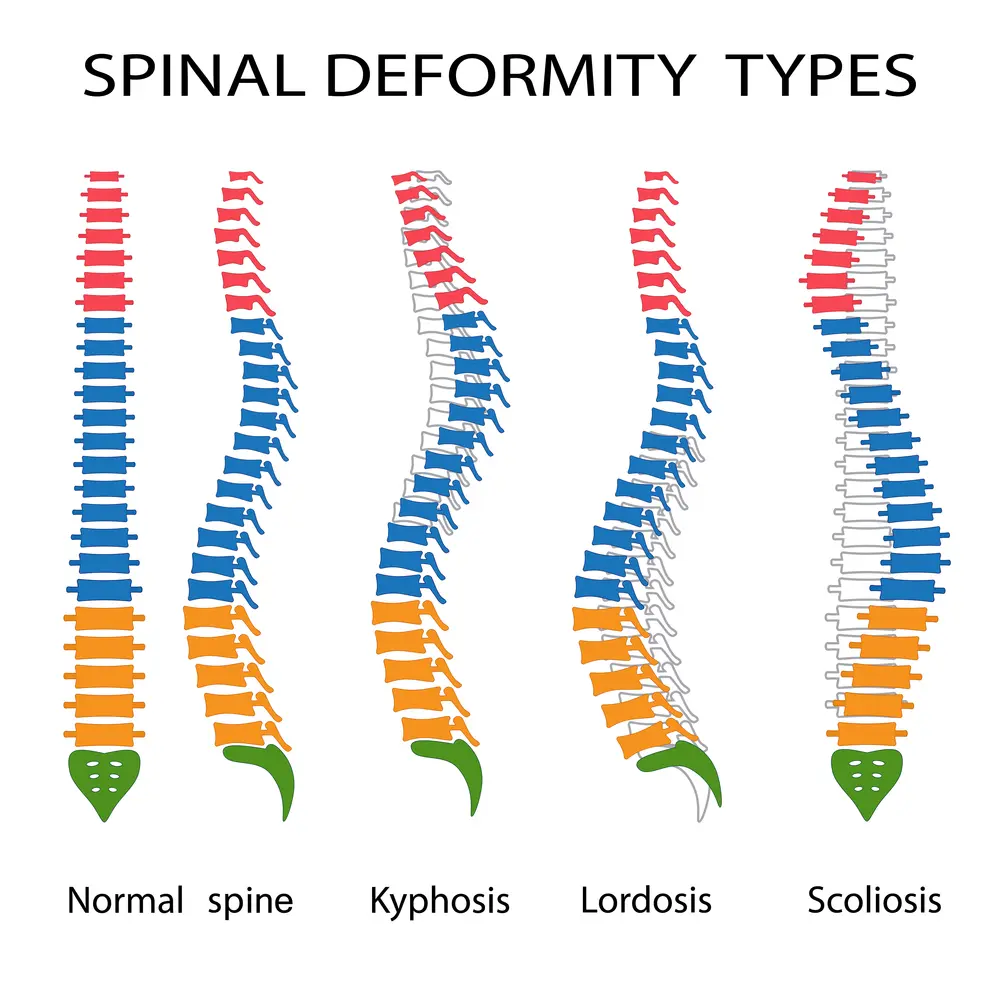
- Visible deformity in the back: Tumor growth can physically alter the spine’s appearance. Growing tumors can become visible through the skin and even change the spine’s curvature, leading to scoliosis, kyphosis, and other deformities.
What Contributes to Their Growth?
Not all types of tumors grow in the same way. For example, benign tumors don’t tend to spread, while malignant tumors – which are commonly seen in metastases or secondary tumors – are particularly aggressive and fast-spreading. Generally, tumor growth is driven by genetic mutations, which cause cells to proliferate unusually quickly and uncontrollably.
Thoracic spine tumors can evolve due to several factors, including genetic predispositions, environmental exposure to cancer-causing chemicals, or underlying conditions like neurofibromatosis. Other contributors include lesions to the thoracic spine and spinal instability.
Understanding these growth mechanisms is critical to obtaining an accurate, timely diagnosis and prompt treatment, which can reduce the risk of complications such as spinal cord compression, nerve damage, or metastasis to other organs.
Lesions on Thoracic Spine
The evaluation of the lesion in the thoracic spine involves many steps. The first step is a detailed medical history where the following is documented: onset of symptoms, duration, location, intensity, aggravating and alleviating factors, and treatment to date. Physical Examination: Evaluation of range of motion, area of tenderness, motor strength, sensation to pinprick, and detailed neurologic examination. Radiographic Studies: Radiographic tests are essential and may include:X-ray: Low-cost and readily available, X-rays provide an image of the bones and can reveal fractures, dislocation, osteoporosis, and deformities like scoliosis and kyphosis. It is often the first-line diagnostic tool used to evaluate spinal conditions. Low amount…
Read More About Lesions on Thoracic SpineSpinal Instability
Spinal instability is a condition that occurs when the spinal column is not able to maintain its normal alignment and function under normal loads. It can be caused by various factors such as trauma, degenerative changes, infections, tumors, or congenital abnormalities. In a stable spine, the bones, discs, ligaments, and muscles work together to support and protect the spinal cord and nerve roots. However, in an unstable spine, the structures that support the spine may be damaged or weakened. This can lead to abnormal movement and excessive stress on the spinal cord and nerves. In most cases, bone and joint problems…
Read More About Spinal Instability- Genetic factors
- Age-related factors
- Environmental factors
- Neurological complications
-Such as balance and coordination issues, bowel and bladder dysfunction, weakness and numbness, chronic pain
Red Flags That Indicate Immediate Medical Attention Is Required
As we have seen above, one of the most dangerous aspects of thoracic spine tumors is the fact that most patients experience nothing more than mild back pain at first, which can be misinterpreted as minor problems like stress or bad posture. This leads to delays in getting a diagnosis and seeking treatment, which, in turn, increases the risk of complications and decreases the survival rate.
That’s where learning to recognize critical symptoms becomes paramount. Some of the telltale signs that may warrant consulting your doctor include:
- Sudden onset of severe back pain: Experiencing abrupt, intense back pain could indicate spinal cord compression or a vertebral fracture. In this case, it is important to seek immediate medical attention to prevent permanent neurological damage.
- Changes in bowel or bladder function: Any sudden loss of control over bowel or bladder functions can signal severe nerve damage. Even if this does not relate to a thoracic spine tumor, it may indicate other serious conditions, like cauda equina. Speak to your doctor immediately to avoid long-term disability.
- Progressive weakness or numbness: Increasing weakness or numbness, especially in the legs, could indicate that your spinal cord or nerve roots are compressed, irritated, or damaged. You may require treatment to prevent further deterioration and restore function.
Diagnosing a Tumor in the Thoracic Spine
If you suspect a spine tumor, nothing is as important as seeking an accurate diagnosis. Not only will this help you and your doctor determine the right approach to safeguard your spine’s health, but it can also save your life if the tumor has been caused by metastases and your disease is in an advanced stage.
Some of the diagnostic tools a specialized healthcare provider will use to determine the cause of symptoms and pinpoint (or rule out) a tumor include:
- Medical history. A review of your medical history is usually the starting point to make a diagnosis, as it provides insights into your lifestyle, symptom history, and background.
- Physical examination. Your doctor may use some tests to determine the presence of neurological problems (e.g.: malfunctioning of nerves) and physical signs of a tumor.
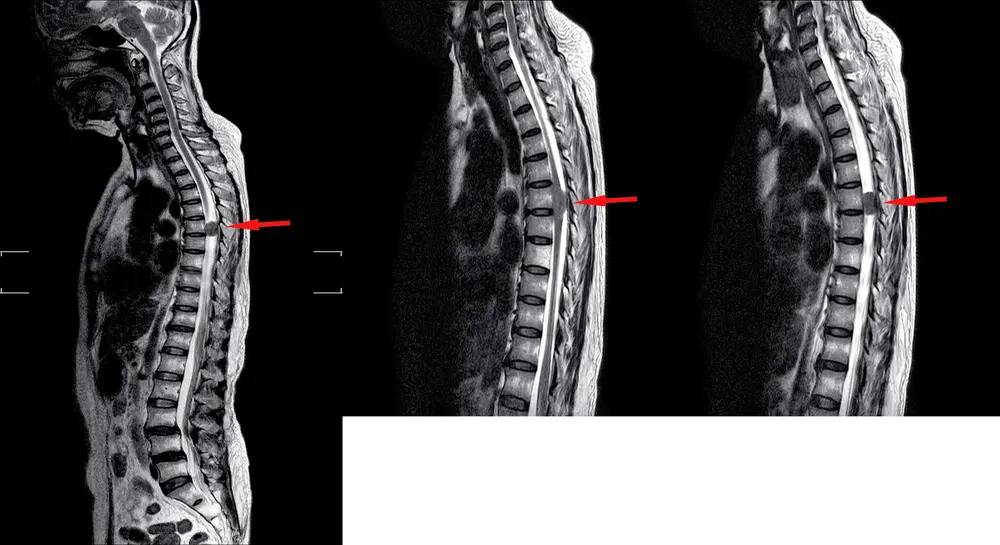
- Imaging tests. Imaging tests can be used to confirm a diagnosis after a hypothesis has been made. There are several options available:
- X-rays. Provide views of the inner aspects of your spine and can help detect bone abnormalities and structural changes, but are not as detailed as other scans.
- CT Scans. Offer detailed cross-sectional images of both hard tissues like bones and soft tissues like blood vessels, to determine whether there’s a circulatory or neurological problem involved.
- MRI scans. Provide high-contrast images of soft tissues, making them particularly useful in visualizing spinal tumors.
- Biopsy procedures. These procedures involve collecting small samples of tissues from the areas affected or the tumor itself to help confirm a diagnosis (i.e.: to determine whether the tumor spreads, and is therefore malignant, or is benign).
Common Treatment Options Available
The treatment recommended to address a thoracic spine tumor will depend on the nature and size of the tumor, as well as other circumstances. However, today, oncology research is advancing in leaps and bounds, introducing new therapies and enhancing existing ones to improve patient safety and clinical outcomes.
For example, although traditional methods like surgery and radiation remain standard options, innovations in minimally invasive techniques and targeted therapies have improved their efficiency and viability. Alongside these options, regenerative medicine and interventional orthopedics are capable of improving patients’ quality of life and well-being while reducing the need for medications or surgery.
Radiation Therapy
Radiation therapy has been one of the first treatments used in the management of cancer, and, although improving significantly, has remained a standard option for decades. This method uses high-energy radiation to target and destroy cancer cells in the thoracic spine. It can be used to shrink tumors, alleviate pain, and prevent tumor growth by damaging the DNA of cancer cells.
Radiation therapy is typically administered over several weeks and involves frequent, brief sessions. Success rates vary based on the tumor’s type and stage, but this therapy frequently plays a significant role in slowing tumor progression. Common side effects include fatigue, skin irritation, and localized pain.
Advances in radiotherapy technology – like intensity-modulated radiation therapy (IMRT) and stereotactic radiosurgery – have enhanced precision, reducing harm to surrounding tissues.
Chemotherapy
Chemotherapy involves the use of drugs – administered intravenously, orally, or directly into the spinal canal – to kill cancer cells or stop them from growing. These medications work by targeting rapidly dividing cells, which include cancer cells, and interfering with cell division processes or DNA replication.
Chemotherapy is often employed alongside other treatments like surgery or radiation for a more efficient, comprehensive approach. Although chemotherapy remains a widely used approach, success rates depend on the specific tumor type and its responsiveness. Additionally, side effects can be severe, including nausea, hair loss, and weakened immune function.
Multidisciplinary Approaches
A multidisciplinary approach usually involves the use of several treatment types and the collaboration of many specialists. It can help improve clinical outcomes and reduce risks, side effects, and complications while offering patients comprehensive and personalized care. Some of the specialties that may come into play include:
- Neurosurgery. Used when the surgical removal of a tumor is possible or to alleviate tumor pressure on the spine.
- Medical oncology. Manages chemotherapy and other systemic treatments.
- Radiation oncology. Manages targeted radiation therapies.
- Orthopedic surgery. Focuses on improving structural support and maintaining spinal stability.
- Physical therapy and rehabilitation. Aids in recovery, improving mobility and strength. It can also help patients live with symptoms like back pain while improving their quality of life.
- Pain management specialists. Help develop strategies to control chronic pain associated with tumors while reducing drug intake, managing medication interactions, and leveraging non-conventional methods for pain reduction (e.g.: acupuncture).
- Genetic counseling. Provides risk assessment and personalized genetic information, helping in tumor prevention among other members of the family. This is particularly important in primary spinal tumors, which can develop due to certain genetic conditions, like neurofibromatosis Type 2 (NF2) and Von Hippel-Lindau disease (VHL).
- Palliative care: Focuses on improving the quality of life for patients living with a spine tumor, often through symptom management and emotional support.
Targeted Therapies
Targeted therapies stem from recent advances in cancer research, and aim to address spine tumors by disrupting specific molecular targets involved in cancer growth and progression. These therapies offer a precise approach, reducing harm to healthy cells and minimizing side effects. Some of the benefits of opting for these treatments – alone or in combination with traditional cancer management methods – include better efficacy and fewer adverse effects.
Here are some of the targeted therapies available today, but it is worth keeping in mind that this landscape is a fast-evolving one, advancing at an unprecedented pace.
- Tyrosine kinase inhibitors (TKIs). These drugs work by blocking enzymes involved in cancer cell signaling and growth.
- Angiogenesis inhibitors. Inhibit the formation of new blood vessels that tumors need for growth.
- Epidermal growth factor receptor (EGFR) inhibitors. Prevent cancer cells from receiving growth signals.
- Immunotherapies. Boost the body’s immune system to recognize and destroy cancer cells, thus blocking tumor growth and helping the body fight back metastases invasion.
- Hormone therapies. Used to block or lower the levels of hormones that fuel certain cancers, such as breast and prostate cancer, or modify how certain hormones behave in the body. These therapies may also be used to ease cancer symptoms.
- PARP inhibitors. These drugs block the enzyme poly ADP ribose polymerase (PARP), which cancer cells use to repair damaged DNA, leading to their death.
- Stem cell treatment. These treatments utilize stem cells to repair or replace damaged tissue in the spine. Stem cells are cells in the body responsible for healing processes, but their levels drop with age or following injury or disease. Regenexx procedures solve this by delivering a high concentration of bone marrow-derived stem cells directly to the damaged area using imaging guidance. This supports the body’s ability to heal naturally.
Surgical Interventions
Surgical interventions are considered when thoracic spine tumors cause severe symptoms, compress vital structures, or don’t respond well to medications. Although the mechanisms of action vary depending on the type of surgery, these interventions generally aim to remove the tumor, alleviate pain, and restore spinal stability.
Common thoracic spine surgery options commonly employed include:
- Tumor resection. This surgery involves the complete or partial removal of the tumor. This procedure is designed to alleviate pressure on the spinal cord and nerves to provide symptom relief.
- Spinal stabilization. Involves placing rods, screws, or cages to stabilize the spine after tumor removal. If the tumor has caused irreversible damage to the spine, this surgery becomes crucial to maintain structural integrity and prevent spinal collapse.
- Decompression surgery. Removes part of the vertebrae to relieve pressure on the spinal cord and nerves, reduce pain, and improve neurological function.
Thoracic spine surgery is technically complex, requiring specialized expertise to minimize risks and maximize outcomes.
Are Surgical and Drug Intervention the Only Options?
Today’s regenerative treatments, such as prolotherapy and platelet-rich plasma (PRP) injections, offer promising results without the invasiveness of traditional surgery or the side effects of drugs.
These techniques leverage the body’s own healing capabilities, focusing on the repair and regeneration of tissues to reduce pain, enhance function, and potentially reverse damage. It is important for patients to explore these emerging alternatives with their healthcare provider when choosing their line of treatment, to access options that are potentially more efficient and less daunting.
Prolotherapy Injections
It has been successful in the treatment of many disorders including neck, shoulder, knee, and ankle pain. Dr. Centeno recently published an article in The Journal of Prolotherapy in which he discusses the use of x-ray guidance with prolotherapy. This ensures that the injection is in the correct place to maximize clinical results. Dr. Centeno discusses the use of prolotherapy for the treatment of neck, knee, sacroiliac joint, ankle, ischial tuberosity, and shoulder pain. At the Centeno-Schultz Clinic x-ray guided prolotherapy is just one of the therapies utilized in the successful treatment of pain. Regenerative injection therapy (RIT) or prolotherapy…
Read More About Prolotherapy InjectionsPRP Injections
PRP is short for platelet-rich plasma, and it is autologous blood with concentrations of platelets above baseline values. The potential benefit of platelet-rich plasma has received considerable interest due to the appeal of a simple, safe, and minimally invasive method of applying growth factors. PRP treatments are a form of regenerative medicine that utilizes the blood healing factors to help the body repair itself by means of injecting PRP into the damaged tissue. In regenerative orthopedics, it is typically used for the treatment of muscle strains, tears, ligament and tendon tears, minor arthritis, and joint instability. There have been more than 30 randomized controlled trials of PRP…
Read More About PRP InjectionsLearn How We Approach Thoracic Spine Care
At the Centeno-Schultz Clinic, we emphasize non-surgical treatment options tailored to your specific condition. Our approach integrates advanced imaging and regenerative therapies designed to harness your body’s healing potential, minimize side effects, and boost your quality of life.
By focusing on minimally invasive techniques and targeting the root cause of your chronic pain, we aim to reduce pain, enhance mobility, and promote long-term health. Discover how regenerative medicine can transform your thoracic spine care at the Centeno-Schultz Clinic.
Our Thoracic Spine Tumor Doctor
If you have been dealing with a Thoracic Spine Tumor and are contemplating surgery, call and set up an evaluation with one of our experts who can further evaluate you and your candidacy for a surgery avoidance.
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate and PRP for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI).
Other Resources for Thoracic Spine Tumor
-
Thoracic Spinal Fusion Recovery Explored
Thoracic spinal fusion is an intricate surgery that involves fusing vertebrae to reduce pain and improve functionality. It is often necessary due to conditions such as scoliosis, spinal fractures, or degenerative disc disease. Recovery from thoracic spinal fusion is a critical phase, requiring careful management to ensure proper healing and restoration of movement. Patients must…
-
The C1 And C2 Vertebrae – What To Know
The C1 and C2 vertebrae, also known as the atlas and axis, are the uppermost bones in the spinal column. They play a crucial role in supporting the skull and enabling head movements. Damage or injury to these vertebrae often leads to pain, limitations to daily activities, and reduced quality of life. Many patients, without…
-
Spinal Fusion Complications Years Later – What You Should Know
Spinal fusion surgery, often performed to alleviate chronic back pain or spinal instability, can lead to complications years later. These may include adjacent segment disease, where nearby vertebrae deteriorate, chronic pain, or hardware failure. Patients might also experience limited mobility and nerve damage over time. Understanding these potential risks is crucial for long-term care and…
-
Spinal Fusion Recovery: What to Expect
Navigating spinal fusion recovery can be a daunting prospect, given its impact on daily life and mobility. Understanding what to expect during this process is crucial for individuals undergoing this procedure. In this article, we’ll explore the typical timeline, challenges, and strategies for managing recovery after spinal fusion surgery, providing insights to help individuals prepare…
-
Back Fusion
Spinal fusion, also known as back fusion, is a surgical procedure designed to help severe spinal instability that causes severe pain or nerve injuries. It involves permanently connecting two or more vertebrae in your spine to eliminate motion between them. This article will delve into the intricacies of spinal fusion, exploring the reasons behind the…
-
Understanding the Thoracic and Lumbar Spines
The thoracic spine and lumbar spine make up a vital nexus of stability and mobility in the human body. In this exploration, we delve into the biomechanics and complexities that define these regions, unraveling their significance in posture, movement, and overall well-being. Understanding the thoracic and lumbar spine not only illustrates the mechanics of our…
-
The L5 Vertebra: Everything You Need to Know
The spine, consisting of 33 individual bones called vertebrae, is divided into five major regions: cervical (neck), thoracic (upper back), lumbar (lower back), sacral (pelvic region), and coccygeal (tailbone). These vertebrae are separated by intervertebral discs, which act as cushions and allow for flexibility in movement. The lumbar spine, also known as the lower back,…
-
Exploring the Lumbosacral Joint: What Should You Be Wary Of?
The L5 S1 joint, or the lumbosacral joint, is a critical joint. It lies between the lumbar segment of the spine and the auricular processes of the sacrum. The L5-S1 joint plays a vital role in transmitting the weight of the body via the sacrum and ilium downwards. The weight is distributed to the femur…
-
Thoracic Spine MRI: What is It?
Are you getting an MRI of your thoracic spine? Get the help you need with the Centeno-Schultz Clinic. Learn what you need to know about this exam. What to expect on your thoracic spine MRI scan? What exactly is an MRI of the thoracic spine? How does an MRI work? What are the risks and…
Want to know more about your condition? Talk to us and we will help you get your back in good shape.