Stabbing, persistent neck pain can be disabling. Patients often turn to neck fusion, a surgical procedure, in the hopes of eliminating the pain. While the procedure aims to address chronic neck pain, it is crucial to recognize potential complications that may arise even years after the surgery. Understanding these complications is essential for patients.
Let’s dig into what a neck fusion is and the complications it may entail.
What Is a Neck Fusion?
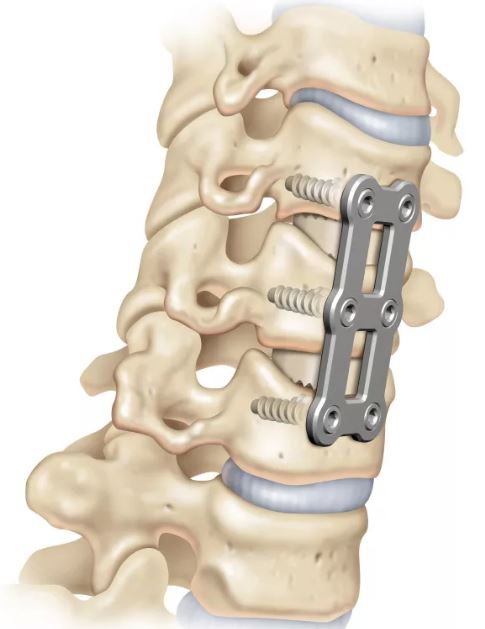
A neck fusion is a surgical procedure where one or more cervical bones (vertebrae) are fused using hardware. The hardware may be placed either in the front (anterior) or the back of the neck (posterior). In many cases, the disc between the fused bones is removed and replaced with bone grafts or a spacer to promote the fusion process.
The procedure aims to stabilize the affected area of the spine, reducing pain and improving overall spinal function. Neck fusion rates are increasing, and from 1997 to 2012 they increased 114% in New York State (1). This statistic underscores the growing acceptance and utilization of neck fusion as a viable treatment for certain neck-related issues.
As the procedure becomes more commonplace, it is essential for both healthcare professionals and patients to be well-informed about the potential complications associated with neck fusion, especially in the years following the surgery.
1. Adjacent Segment Disease
Adjacent segment disease (ASD) is a common complication of neck fusion, with an incidence of 21% (8). The neck discs are designed to absorb the forces of daily living. Fusing one or more discs results in additional forces being placed on the disc and facet joints above and below the fusion.
This additional pressure results in wear and tear and degeneration, oftentimes requiring additional surgery. See our video below:
2. Pseudoarthrosis
Failure of the bones to fuse is called non-union or pseudoarthrosis. This is bad, as the intended surgery has failed and now there is instability in the neck. The incidence of non-union is striking and in one study was found to be 52% (2).
The treatment for non-union is terrible as it involves another surgery where the fusion is revised, and oftentimes the fusion is extended up or down an additional level.
3. Dysphagia
Difficulty swallowing is called dysphagia and can occur after neck fusion. The incidence of dysphagia within one week after surgery varies from 1 to 79% in the literature (3). Difficulty swallowing can compromise calorie and fluid intake, and healing.
4. CSF Leak
The dura is the outermost membrane that covers the brain and spinal cord. This important membrane can be punctured during surgery causing a leak of cerebral spinal fluid (CSF). The incidence ranges from 1-17% (4).
Severe headache is a common symptom of a dural leak. If left untreated it may lead to infection, brain abscess, and bleeding (5).
5. Nerve Damage
Nerves can be damaged during surgery and the incidence varies from 0.18% to 2.6% (6). Nerve injury can include existing nerves as well as the spinal cord itself. Patients who undergo surgery for nerve pain may awaken after surgery with new-onset arm, face, throat or lower / upper extremity pain. Surgical approach is either through the front or back of your neck with majority going through the anterior or front of your throat. This places multiple nerves and blood vessels at risk of being injured. Just to name a few: Vagus nerve, brachial plexus, spinal cord, or recurrent laryngeal nerve. Also major blood vessels such as carotid artery and vertebral arteries (these supply your brain and spinal cord) so damage to these can cause a stroke / nerve damage due to poor blood flow!
6. Infection
Infection is a devastating complication and was found to occur in 16.6% of patients in a recent study (7). Infections can involve the skin, muscle, or bone. Treatment involves antibiotics and wound care, and sometimes also involves skin grafts. A recent study showed that 47% of its patients required additional surgery for wound care and skin grafting.
7. No Reduction in Pain After Neck Fusion Surgery
Inadequate symptom relief after the surgery: despite surgery and rehabilitation, some patients do not get better after surgery. In a recent study one year after neck fusion, only 39% of patients were able to return to work (9).
8. Alterations in Spinal Curve
Changes in the spinal curve: in a recent study, 48 patients who had undergone neck fusion had whole spine X-rays at 1,3,6, and 12 months after surgery. The X-rays noted that changes in the neck curve from surgery impacted the angles of the tailbone and pelvis (10).
9. Anesthesia Complications
Anesthesia complications in neck fusion surgeries can pose significant challenges.
First, patients may experience adverse reactions to anesthesia medications, leading to complications such as allergic reactions or respiratory distress.
Second, difficulties in airway management during intubation may arise, particularly in patients with pre-existing airway issues.
Third, nerve injuries may occur due to positioning during surgery or compression by equipment, resulting in neurological deficits. Fourth, inadequate pain control during the postoperative period can impact patient comfort and recovery.
Additionally, there is a risk of complications associated with the use of neuromuscular-blocking agents, potentially leading to prolonged paralysis or muscle weakness. Lastly, patients with underlying health conditions may face increased vulnerability to anesthesia-related complications, necessitating thorough preoperative assessments and careful monitoring throughout the surgical process.
10. Lung Problems
Neck fusion surgery can potentially lead to lung problems, primarily associated with anesthesia and surgical procedures. First, postoperative atelectasis, a partial or complete collapse of the lung, may occur due to restricted lung expansion during surgery and the use of anesthesia.
Second, pneumonia can develop as a complication, particularly if there is difficulty clearing secretions or impaired respiratory function after the surgery. Third, neck fusion patients may experience respiratory distress syndrome, characterized by inflammation and fluid accumulation in the lungs.
Fourth, the risk of aspiration pneumonia is heightened during intubation and anesthesia administration, especially if there are issues with proper airway management. Fifth, pre-existing respiratory conditions, such as chronic obstructive pulmonary disease (COPD), may be exacerbated, leading to increased respiratory challenges post-surgery.
Lastly, deep vein thrombosis (DVT) and pulmonary embolism are potential complications that can affect lung function due to decreased mobility after the surgery. Vigilant monitoring and appropriate postoperative respiratory care are essential to mitigate these risks.
Why Do These Complications Occur?
It’s important to acknowledge that while all neck fusion surgeries inherently carry risks and complications, certain factors may contribute to the heightened rate of occurrence:
- Your surgeon’s capacity and ability to operate: Firstly, the surgeon’s skill, experience, and overall capacity to perform the procedure play a crucial role. A surgeon’s expertise in navigating potential challenges during surgery can significantly impact the outcome and reduce the likelihood of complications.
- Your disc and physical condition: Secondly, the condition of the patient’s discs and their physical health at the time of surgery is a significant determinant. Pre-existing conditions, such as the degree of degeneration in the spinal discs, can influence the complexity of the procedure and the potential for complications.
- Your lifestyle: Lastly, a patient’s lifestyle and overall health are contributing factors. Factors such as smoking, obesity, or a sedentary lifestyle can increase the risk of complications during and after neck fusion surgery. These lifestyle elements may affect the healing process, the body’s response to anesthesia, and the overall success of the surgical intervention.
Is There Any Alternative Non-Surgical Option To Treat Neck Pain?
Absolutely!
At the Centeno Schultz Clinic, autologous ortho-biologics (platelets and BMC) are precisely injected into the neck using X-ray and ultrasound guidance. The injections are challenging and cannot be performed by your surgeon, chiropractor, or physician assistant. To watch a Centeno-Schulz clinic injection, click on the video below.
Regenexx Cervical Spine Regenerative Procedures
Regenexx may offer alternatives to traditional surgical interventions for conditions like degenerative disc disease, herniated discs, or other spine-related issues. These procedures often involve injecting concentrated platelets or bone marrow concentrate directly into the affected area to promote healing and regeneration.
Platelet-Rich Plasma (PRP)
PRP for cervical radiculopathy has become very popular for patients with neck pain. It involves using platelet-rich plasma from the patient, which the doctor injects into the damaged areas via a precise image-guided procedure.
This PRP concentrate is rich in platelets and platelet growth factors that can stimulate other cells to repair and grow, promoting local tissue healing.
The best thing about PRP is that it has very few side effects or complications when compared to ACDF. It is also a quicker procedure and encourages the body to heal itself with platelet growth factors.
At Centeno-Schultz, we continue to innovate and have advanced PRP to now platelet lysate (currently in our 4th generation) for these advanced cervical procedures! Platelet lysate provides multiple benefits as compared to regular PRP:
- Safer to use as compared to PRP in the cervical spine, PRP are stripped of the platelet shells and isolated concentration of immediate-release growth factors. With over 150 high quality randomized controlled trials showing much better than traditional injections such as high dose corticosteroids
- Our unique processes create a much higher quantity of growth factors which provides a greater probability of success using a patented process via our flexible lab platform. You can learn more about it here.
Can You and Should You Take a Follow-Up Surgery in Case of Complications?
The decision to undergo a second surgery following complications from neck fusion, such as adjacent segment disease (ASD), is a complex and individualized consideration. The occurrence of complications like ASD may necessitate additional surgical intervention, but the decision is contingent upon various factors, chiefly the surgeon’s judgment and the patient’s specific condition.
The decision-making process involves an assessment of the severity of complications, the impact on the patient’s quality of life, and the potential benefits of a second surgery. Surgeons evaluate factors such as the overall health of the patient, the extent of spinal degeneration, and the presence of other underlying conditions that may influence the surgical outcome.
The surgeon’s expertise and experience play a pivotal role in determining the appropriateness of a second surgery. Experienced surgeons can navigate the complexities of revision procedures with greater skill and precision, potentially minimizing risks and optimizing outcomes.
Patient-specific factors, including overall health, lifestyle, and willingness to undergo further intervention, also weigh heavily in the decision-making process. Open communication between the patient and the surgeon is crucial to ensure informed consent and realistic expectations regarding the potential outcomes and risks associated with a second surgery.
In conclusion, while a second surgery may be considered in the face of complications arising from neck fusion, the decision is highly individualized and depends on the collaborative assessment of the surgeon and the unique circumstances of the patient.
Looking for more information on the available treatment options for your condition? Let us help you safely manage your pain.