When back pain becomes severe, surgery is often recommended. What is a Laminectomy? What is Postlaminectomy Syndrome? What are the Symptoms of Postlaminectomy Syndrome? What are the complications of Laminectomy surgery? What is the treatment for Postlaminectomy syndrome? What natural regenerative options exist? Let’s dig in.
What is a Laminectomy?
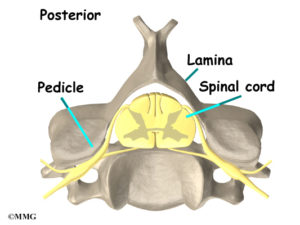
The lamina is a thin section of bone in the spine that provides support and protection for the spinal cord. In medicine, the term “ectomy” refers to cutting or removal of a structure. So a Laminectomy is a spine surgery that removes the lamina which is intended to reduce ongoing low back pain. It is usually performed to relieve pressure on the spinal cord.
What is Postlaminectomy Syndrome?
Postlaminectomy syndrome (PLS) is a clinical condition in which pain continues after laminectomy surgery (1). It is also called failed back surgery. The incidence ranges between 10% and 40% (2). The pain may be the same as prior to the surgery or increased and often times there are new symptoms such as numbness, tingling, and weakness. Postlaminectomy syndrome patients with nerve pain experience intense levels of pain, lower quality of life, greater disability, and higher rates of unemployment (3).
Who is at risk for PLS? Patients with poor psycho-social wellbeing (4) history of smoking, obesity, and prior spinal surgery (5).
What are the Symptoms of Postlaminectomy Syndrome?
Common symptoms that occur with the Postlaminectomy Syndrome include:
- Low back pain
- Radiating leg pain
- Intense muscle spasms
- Leg weakness
- Buttock pain aggravated by sitting
- Complications from Laminectomy Surgery
Laminectomy surgery is associated with a number of complications. The most common include nerve damage, blood clots, spinal fluid leak, bleeding, infection, and escalation in pain. Another important complication is destabilizing the spine. Laminectomy can create an unstable spine since important ligaments, tendons, and muscles are damaged or removed during surgery. A case in point is JM who presented to our clinic with complaints of ongoing pain after Laminectomy. His MRI is significant for a very large hole created by surgery. The images below show the issue.
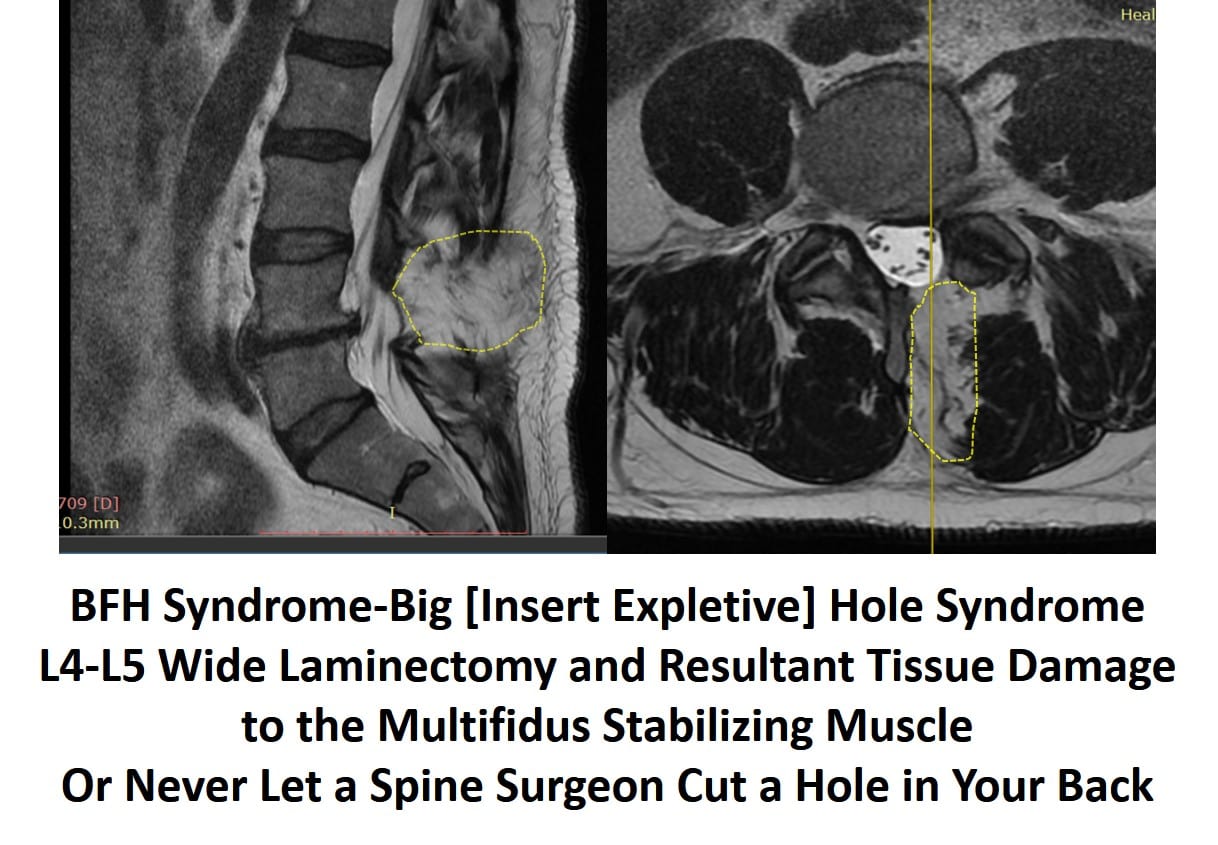
On the left-hand side, you see a side image of the spine. Note that the yellow-dashed line represents the hole caused by surgery. You can easily see dark bones and muscles above and below the hole, but that area looks white. Now, look at the image on the right. This is a view looking down on the tissues (axial or “saw you in half” view). The yellow-dashed line again outlines the hole. You see the dark low back muscles surrounding the white void. In fact, the hole is exactly where the critical stabilizer of the low back, called the Multifidus, should live. Meaning, at this level that muscle has been obliterated, causing serious problems and spinal instability.
Why is the Multifidus muscle so important? See the video below for more information:
What Is the Treatment for Postlaminectomy Syndrome?
The best way to treat postlaminectomy syndrome is to avoid having low back surgery in the first place. There are a number of reasons why patients have back pain following Laminectomy surgery which include disc herniation, irritation of nerve root, infection, scar tissue, and adjacent segment disease. Regrettably, the problem that the Laminectomy was intended to fix may not have been the source of the pain. Traditional treatment options for PLS include the following.
- Conservative Care: PT, chiropractic care, Pilates, behavioral modification, and biofeedback.
- Medicine: Multiple medications have been tried which includes muscle relaxants, narcotics, anticonvulsants, tramadol, and NSAIDs. All have side effects which can include addiction.
- Repeat Surgery: Clinical benefit is limited as no more than 30%, 15% and 5% of patients experience a successful outcome after second, third and fourth surgeries respectively (7)
- Spinal Cord Stimulation: An implanted device into the spine that reduces the pain by sending electrical signals to the spinal cord. Multiple studies have demonstrated reduced pain in patients with spinal cord stimulation (8)
Are there natural regenerative options? Yes! Look up our Perc-FSU procedure – the trusted alternative to spine fusion.
PRP and Stem Cell Treatment Options
PRP contains multiple growth factors that can increase blood flow, stimulate healing, strengthen ligaments, and reduce nerve irritation. Stem cells can accelerate healing and orchestrate cells from other parts of the body to assist in that repair. In 2005, the Centeno-Schultz Clinic was the first clinic in the world to inject stem cells into the lumbar disc.
We are experts in the treatment of spine and nerve injuries. A SANS approach is utilized that is comprehensive in nature and provides a better outcome for patients. In our 2017 paper, we demonstrated that PRP epidural injections were more superior to steroid injections. All procedures are performed under x-ray or ultrasound guidance, or both, in a max COVID-protected clinic.
In Conclusion
The lamina is a thin section of bone in the spine that provides support and protection for the spinal cord. Laminectomy is a spine surgery that removes the lamina which is intended to reduce ongoing low back pain. Postlaminectomy syndrome (PLS) is a clinical condition in which pain continues after having Laminectomy surgery. Symptoms include low back pain, radiating leg pain, intense muscle spasm, and leg weakness. Complications associated with Laminectomy include nerve damage, bleeding, infection, and spinal instability. The best treatment is to avoid low back surgery in the first place. Traditional treatments include conservative care, medications, repeat surgery and spinal cord stimulation. PRP and stem cells are natural treatment options that do not alter the structure or stability of the spine.
1. Follett KA, Dirks BA. Etiology and evaluation of the failed back surgery syndrome. Neurosurg Q. 1993;3:40–59.
2..Sebaaly A, Lahoud MJ, Rizkallah M, Kreichati G, Kharrat K. Etiology, Evaluation, and Treatment of Failed Back Surgery Syndrome. Asian Spine J. 2018;12(3):574-85.
3. Chan CW, Peng P. Failed back surgery syndrome. Pain Med. 2011;12(4):577-606.
4.Nachemson AL. Evaluation of results in lumbar spine surgery. Acta Orthop Scand Suppl. 1993;251:130-3.
5. Sanden B, Forsth P, Michaelsson K. Smokers show less improvement than nonsmokers two years after surgery for lumbar spinal stenosis: a study of 4555 patients from the Swedish spine register. Spine (Phila Pa 1976) 2011;36:1059–1064.
6. Phillips FM, Cunningham B. Managing chronic pain of spinal origin after lumbar surgery: the role of decompressive surgery. Spine (Phila Pa 1976) 2002;27:2547–53.
7. Nachemson AL. Evaluation of results in lumbar spine surgery. Acta Orthop Scand Suppl. 1993;251:130-3.
8.Kumar K, Taylor RS, Jacques L, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomized controlled trial in patients with failed back surgery syndrome. Pain. 2007;132:179–188.