Tarsal Tunnel Syndrome
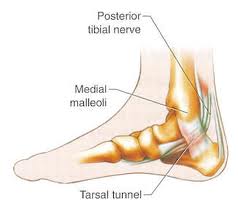
Carpal tunnel syndrome is compression of the median nerve at the level of the wrist with resultant hand and wrist pain. Tarsal tunnel syndrome (TTS) – also called tibial neuralgia – is the equivalent in the ankle.
What is Tarsal Tunnel Syndrome (TTS)?
TTS is compression of the tibial nerve as it passes through the tarsal tunnel at the ankle. The tarsal tunnel is located behind the medial malleolus, the bump on the inside of the ankle.
Causes of TTS
TTS can be caused by a variety of diseases and circumstances that strain or compress the tibial nerve, including:
- Flat feet
- Fallen arches
- Inflammation caused by an ankle sprain
- Arthritis or diabetes – swelling of feet
- Bone spur
- Ganglion cyst
Symptoms of Tarsal Tunnel Syndrome
Patients typically complain of pain, numbness, tingling, or burning sensation in the foot, including in the big toe and the first two to three toes.
Some patients complain of pain at the ball of the foot that is often worse when they are wearing shoes. The symptoms often occur during the night and may be more noticeable after resting or sleeping. Symptoms can also worsen during prolonged standing, walking, or any other activity in which the ankle is bearing weight.
Treatment Options for TTS or Tibial Neuralgia
At the Centeno-Schultz Clinic, the first step is a complete history and thorough examination. Some patients may have a Tinel’s sign. Ultrasound examination provides a dynamic picture of the structures within the tarsal tunnel including scar tissue and tendon irritation. Hydrodissection is a non-surgical treatment option for tarsal tunnel syndrome in patients who have failed conservative therapy.
Conservative Therapy
- Physical therapy
- RICE – rest, ice, compression, elevation
- Medication
Surgery
Surgery for tarsal tunnel syndrome is performed endoscopically, and the flexor retinaculum is released and reconstructed (1).
Regenerative Treatment Options
- Hydrodissection with prolotherapy
- Hydrodissection with platelet-rich plasma
Nerve Hydrodissection
Nerve Hydrodissection is a medical procedure that aims to free up scar tissue or adhesions on a given peripheral nerve. The procedure utilizes ultrasound guidance to visualize both the needle and the targeted nerve. Medication is then injected through the needle to free up the scar tissue. Nerve Hydrodissection is a minimally invasive treatment option for many peripheral nerves that are compressed or entrapped by scar tissue.Pain is an uncomfortable and at times painful sensation. It varies significantly from patient to patient. There are many different types of pain which include inflammatory, nociceptive, and neuropathic. Neuropathic pain is pain that arises from nerve compression or injury.
Read More About Nerve HydrodissectionNSAIDs
The other day I was evaluating a patient and reviewing the treatment options for their spine condition. After discussing prior treatments, we got to the topic of medications taken for pain relief. She explained that she mainly utilized anti-inflammatory (NSAID) medications and then she told me to hold much she takes and has been for many years…..she takes close to 2 grams (2000 milligrams) on a daily basis which equated to about 9-10 capsules of medication per day. I was shocked, considering she was pre-diabetic and with high blood pressure plus the kicker of it is that her PCP (primary care physician) is ok with this…
Read More About NSAIDsPRP for Nerve Damage
Peripheral nerves are comprised of various combinations of motor, sensory, and autonomic neurons. Nerve injuries are a common condition with a broad range of symptoms depending on the severity of nerve damage which presents various challenges to patients, ranging from mild discomfort to life-long impairment. PRP for nerve damage has been shown to be effective. Let’s dig in. Nerve injuries can be classified based on the severity of damage and which structures in the nerve have been damaged. The most severe case is the complete transection of the nerve, called neurotmesis. The most common is neuropraxia from acute or chronic compression of the nerve.
Read More About PRP for Nerve DamageOur Doctors Who Treat Tarsal Tunnel Syndrome

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreMore Resources for Tibial Neuralgia
-
Craniocervical Instability and Vagus Nerve Compression
Craniocervical instability (CCI) occurs when the supportive muscles and ligaments in the upper cervical spine become ‘loose’ or ‘lax’. The importance and complexity of the vagus nerve is highlighted in its name. Vagus is the Latin word for ‘wandering’ and, as the name suggests, the vagus nerve travels widely throughout the body, resembling the root…
-
Transverse Cervical Artery
The transverse cervical artery (TCA) is a branch of the thyrocervical trunk, which itself is a branch of the first part of the subclavian artery. These arteries are part of the larger arterial network that supplies blood to the head, neck, and upper limbs. Understanding the anatomy and function of arteries like the TCA is…
-
Exploring the Anatomical Structures of an Ulnar Nerve
The human body is a marvel of intricate design, and its functioning relies on a network of complex systems. Among these, the nervous system serves as the communication highway, transmitting signals that enable us to move, feel, and interact with the world around us. One crucial component of this neural network is the ulnar nerve,…
-
Guyon’s Canal Treatment Options
Growing up in South Florida, I never knew what it was like to have different seasons – we basically had hot, hotter, and blistering hot! But now being in Colorado for many years, I understand the transitions from winter to spring. It means that its time to put away my snowboard and dust off the golf…
-
PRP for UCL Injury – PRP Injections for UCL Tear
Dr. Pitts Talks About PRP for UCL Injury as an Alternative to Tommy John Surgery Transcript Hi everybody. This is Dr. John Pitts with the Centeno-Schultz Clinic, where we lead and invented much of the field of Interventional Orthopedics and regenerative medicine. Mainly we treat most musculoskeletal and orthopedic problems with injections of your own…
-
Non-Surgical Peripheral Nerve Treatment
Nerves typically become injured via compression. They get compressed in fascial layers. The compression usually happens through scar tissue formation, bone spurs, and tight muscles can compress the nerves. Tight muscles can also push the nerves into a bony prominence, or get stretched around a bone. So What Is a Hydrodissection? Non-Surgical Peripheral Nerve Treatment…
- Yoshida A, Okutsu I, Hamanaka I. Endoscopic tarsal tunnel syndrome surgery using the Universal Subcutaneous Endoscope system. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015;3:1-5. Published 2015 Nov 2. doi:10.1016/j.asmart.2015.09.001