Thoracic Outlet Syndrome
Causes, Symptoms, Treatments, & Other Resources
New Treatment Option for Thoracic Outlet Syndrome
If you’ve had symptoms like numbness or tingling in your hands or arm, aches or pain in your shoulder or neck, a weakening grip, or the muscles in your hand shrinking, you may have been told you have thoracic outlet syndrome.
What Is the Thoracic Outlet?
The thoracic outlet is an area around the collar bone where the nerves that come from your neck meet up with the blood vessels from your heart and together supply the entire upper extremity (shoulder and arm). These blood vessels (subclavian artery and vein) and nerves (brachial plexus) travel from the base of your neck to your arm pit (axilla) and is considered the “thoracic outlet” (1). Now that you know what the thoracic outlet is, what is thoracic outlet syndrome?
What is Thoracic Outlet Syndrome (TOS)?
Causes of the different Thoracic Outlet Syndrome
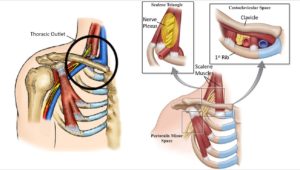
TOS symptoms are positional intermittent compression of the brachial plexus and/or subclavian blood vessels. There are 3 areas that can cause the compression (2).
1. Scalene triangle – Muscle spasms or chronically tight scalene muscles can compress the nerve plexus as the nerves travel through them.
2. Costoclavicular Space – this narrow space can compress the nerves or blood vessels in several ways
3. Pectoralis Minor Space – typically poor posture leads to chronic tightness of this muscle and muscle spasms that in turn compress the structures under the muscle.
Is TOS Serious?
Like most syndromes, there is a variety from very mild cases to life-threatening. TOS is a group of symptoms in the chest, neck, shoulder, and arms and can be broken into 3 different types:
1. Neurogenic thoracic outlet syndrome (nTOS).
This most common type of thoracic outlet syndrome is characterized by compression of the brachial plexus. The brachial plexus is a network of nerves that come from your spinal cord and control muscle movements and sensations in your shoulder, arm, and hand. This is considered the most common type of TOS, making up 95% of all cases. This creates a numb feeling in the arm. It can be isolated to a single nerve or multiple nerves (3).
2. Vascular thoracic outlet syndrome (vTOS).
This type of thoracic outlet syndrome occurs when one or more of the veins (venous thoracic outlet syndrome) or arteries (arterial thoracic outlet syndrome) under the collarbone (clavicle) are compressed. Which can lead to extremity swelling, cyanosis (blue discoloring of the skin), and possibly deep venous thrombosis (blood clot in arm) (4).
3. Nonspecific-type thoracic outlet syndrome.
This type is also called disputed thoracic outlet syndrome. Some doctors don’t believe it exists, while others say it’s a common disorder. People with nonspecific-type thoracic outlet syndrome have chronic pain in the area of the thoracic outlet that worsens with activity, but a specific cause of the pain can’t be determined (5).
· Muscle wasting (Gilliatt-Sumner hand)
· Numbness or tingling in your arm or fingers
· Pain or aches in your neck, shoulder or hand
· Weakening grip
Common Symptoms of Thoracic Outlet Syndrome
Arm Pain at Night
Arm pain at night can be miserable. The pain can interrupt your sleep and erode your quality of life. Irritability becomes increasingly more common. What are the causes? When should I worry about it? What are the treatment options for arm pain at night? The neck is composed of 7 boney building blocks numbered 1- 7. Sandwiched between the bones is a disc that functions as an important shock absorber. The cervical discs are susceptible to injury due to trauma, degeneration, repetitive motion, and surgery. Common disc injuries include disc bulges, and herniations. The injured disc can compress or irritate one or more nerves resulting in arm pain at night. It can…
Read More About Arm Pain at NightArm Throbbing
In many patients, irritated neck nerves don’t present as a symptom in the neck. In fact, sometimes the only symptoms of irritated nerves in the neck occur in the arm muscles, as either tightness, throbbing, or both. While the arm throbbing might be frustrating as it’s happening, you might not think a whole lot about it, especially if it only happens on occasion. However, ignoring it is not a good idea since it is often a warning signal of a bigger problem in the neck. These body connections occur all the way back to when we were a fetus, like the neck, shoulder, and arm.
Read More About Arm ThrobbingFeeling Of Pins And Needles In Fingers
Are you experiencing the sensation of pins and needles in your fingertips? This is a common symptom of cervical radiculopathy. Although many conditions can cause pins and needles, if it is accompanied by neck pain, then cervical radiculopathy would be at the top of the diagnostic list. Cervical radiculopathy also referred to as a “pinched nerve.” is a medical syndrome that occurs when a nerve root in the neck ( cervical spine) becomes compressed or irritated leading to symptoms that include pain, numbness, tingling, and potentially weakness. It occurs in about 85 people per 100,000 (1). Read this post to find out more about cervical radiculopathy and how it can cause pins and needles in your fingertips.
Read More About Feeling Of Pins And Needles In FingersLeft Arm Numbness
Treatment depends upon the underlying cause of the arm numbness. Left-arm numbness is a warning sign that requires attention. As noted above unexplained numbness requires immediate attention. At the Centeno-Schultz Clinic, we are experts in the treatment of left-arm numbness due to cervical nerve irritation, cervical stenosis, thoracic outlet syndrome, and peripheral nerve injuries. When appropriate first-line treatment should involve conservative care including physical therapy and stretching. Steroid injections should be avoided as they are toxic to orthopedic tissue and can accelerate damage. Surgery for Cervical Stenosis and Thoracic…
Read More About Left Arm NumbnessNerve Pain in the Thoracic Spine
The thoracic spine is the part of the spine below the neck (cervical spine) and above the low back (lumbar spine). It is often referred to as the mid back. Nerves exit the thoracic spine at each level and can become irritated, compressed or injured, resulting in pain and dysfunction. This is commonly referred to as thoracic radiculopathy or pinched nerve.
Read More About Nerve Pain in the Thoracic SpineShoulder Pain Radiating Down Arm to Fingers
Common Cervical Radiculopathy symptoms include neck pain, arm pain, shoulder pain radiating down arm to fingers, numbness, tingling, and weakness. Cervical Radiculopathy is a clinical condition in which a nerve or nerves in your neck become irritated or compressed. It is also known as ” a pinched nerve,” The causes are discussed below. It can affect individuals of any age with peak prominence between ages 40-50 years of age. Cervical Radiculopathy is due to spinal nerve inflammation, irritation, or compression. The most common causes of Cervical Radiculopathy are: Disc Injury – The disc is an important shock absorber. Unfortunately, it is susceptible to injury.
Read More About Shoulder Pain Radiating Down Arm to FingersShoulder Pain When Reaching Across Body
Shoulder pain can make simple chores almost impossible. Have you ever reached for an object high on a shelf only to have pain that takes your breath away? What causes shoulder pain when reaching across the body? What is shoulder impingement? What does shoulder impingement feel like? Can a shoulder X-ray show shoulder impingement? What are the treatment options for shoulder pain when reaching across the body? ulder impingement and rotator cuff injuries are among the most common causes of shoulder pain (1). Both can cause shoulder pain when reaching across the body. Shoulder impingement is a painful condition in which the bursa and muscles of the shoulder are pinched or compressed.
Read More About Shoulder Pain When Reaching Across BodyShoulder Pain When Sleeping
There are several reasons why shoulder pain at night occurs or is aggravated; The common explanations include: Sleep typically involves a static position lasting hours at a time with little or no movement. Sleeping on your side places additional pressure on the tendons and bursa of the shoulder. Sleep can cause muscles and tendons to settle in a slightly different position resulting in additional pressure and reduced blood flow. Identifying the underlying problem is important! This allows therapy to focus exclusively on the exact problem or problems. When appropriate conservative care is always the first line of treatment. Focus is typically on strengthening and improving range of motion.
Read More About Shoulder Pain When SleepingThoracic Spine Pain
Simply put thoracic spine pain is pain that arises from the thoracic spine. It may be acute or chronic. It may be constant or intermittent. It may be mild or can be so severe as to take your breath away. To better understand thoracic spine pain please review the sections below. The thoracic spine is that part of the spine that is sandwiched between the neck and low back. Many refer to it as the middle section of your spine. It starts at the base of your neck and ends at the bottom of your ribs. The thoracic spine is the longest region in the spine.
Read More About Thoracic Spine PainTingling Sensation in the Hands
Have you ever felt the sensation of a thousand tiny pins and needles pricking your hands or the subtle, electric tingling that runs down your fingers like a gentle current? Tingling sensations in the hands are more common than you might think and can be triggered by a multitude of factors, from temporary nerve compression to chronic medical conditions. While often dismissed as a momentary inconvenience, this seemingly innocuous tingling can sometimes be a signal from your body, a signpost pointing to underlying health concerns. In this article, we delve into the intriguing world of tingling sensations in the hands, unraveling the causes, potential implications, and, most importantly, what you can do to address them.
Read More About Tingling Sensation in the HandsHow Do You Diagnose TOS?
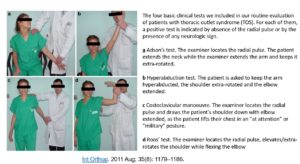
Simply listening to a patient’s history and completing a physical examination is all that is needed to diagnose TOS. But more involved imaging such as X-rays, diagnostic ultrasound, MRIs, EMG (nerve conduction test) are used to rule out the underlying issue (2).
How Long does It Take to Recover from TOS?
Recovery depends on the severity of the syndrome and response to treatment. Thoracic Outlet Syndrome can resolve in a matter of weeks to months or can become chronic and last many years before getting proper treatment.
Can Thoracic Outlet Syndrome Be Cured?
Conservative options for TOS include modification of behaviors by avoiding activities that aggravate symptoms, and arm positions, along with physical therapy programs that strengthen the muscles of the pectoral girdle and help to restore normal posture (6, 7). TOS can be treated successfully with simple physical therapy. A paper by Dobrusin comments on how dysfunctional area treatment can, “decrease muscular tone in the scalene muscles, allow the first rib to become more mobile, and open up the interscalene triangle” (8). Success can vary, as 50% to 90% of patients respond well to conservative care.
Treatment Options
Some patients respond well to medications for this. Pharmacologic interventions often provide symptomatic relief and primarily include analgesics (NSAIDs and/or opioids) for nerve pain, as well as muscle relaxants, anticonvulsants (anti-seizure drugs), and/or antidepressants (9). The downside, if these medications help then you may be on them for the rest of your life!
Additionally, injection of local anesthetic, steroids, or botulinum toxin type A into the anterior scalene and/or pectoralis muscle has demonstrated varying levels of success in observational studies (10). BUT failed to demonstrate any benefit in a larger randomized control trial (11).
If failed those and continues to be debilitating, the patient will be referred to cardiothoracic surgeons for a first rib resection with scalenectomy. Utilizing the “when in doubt, take it out” mentality by removing the rib and muscles that are creating the compression! But do you need your first rib and scalene muscles and are these surgeries safe?
There is limited research on long-term follow-up outcomes for these patients. In the short term, studies show 6.7% of patients have postoperative bleeding requiring thoracentesis (draining the bleeding from your lungs) or video-assisted thoracoscopic evacuation (small camera into the lung to find the bleeding) of hemothorax (12, 13). Other risks with this type of surgery are wound infection, lymph leak, brachial plexus injury, winged scapula (from injury to the long thoracic nerve), or paralyzed hemidiaphragm (from injury to the phrenic nerve). Hosseinian showed that nerve injuries to the nerves that are being decompressed can be as high as 9% (13, 14)!
NEW Percutaneous-Orthobiologic Approach
Combining the best of interventional orthopedic techniques with the most advanced ortho-biologics can help reduce the conversion of patients that are referred to surgery by a significant number.
We have seen excellent results utilizing a SANS approach with a multi-faceted treatment. Clinic on the link to get a better understanding of the utilization of the SANS approach to treating orthopedic conditions.
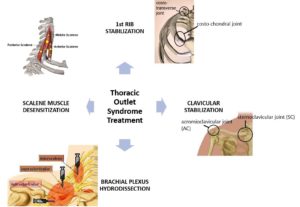
Here is an ideal treatment for TOS:
While this treatment is an excellent alternative to more invasive surgeries, these injections are not without risks and need to consider who is able to perform these injections safely and effectively. While many physicians still utilize a “feel and poke” (blind) method for injecting. Please be aware, the risk of complications from blind injections can increase complication rates drastically. The advent of musculoskeletal ultrasound and utilization of fluoroscopic guidance has made it possible to visualize soft tissue and boney structures allowing us to avoid the things we don’t want to inject (nerves, blood vessels) and directly inject the ligament or place injection around a nerve without damaging the nerve! These treatments are highly advanced injections that require advanced training to do these safely – here is a video done by Dr. Centeno explaining interventional orthopedics
Upside…
There are thousands of patients that suffer from TOS and up to 50% may require surgery. We have created a treatment option that is far less invasive and involves far less risk of serious complications with the goal to improve symptoms and overall function without the need for surgery. If you have been diagnosed with TOS and considering alternatives to surgery, feel free to contact us. We’re happy to discuss and evaluate you further to see if you are a good candidate for this new treatment option!
A Deep Dive Into the Treatment Options
Prolotherapy For Thoracic Pain
Prolotherapy is an injection based regenerative therapy used in the treatment of ligament, tendon, muscle and spine injuries. It is minimally invasive and involves the injection of an irritant such as dextrose into the damaged or painful area. The injected irritant stimulates a delayed or frozen healing cycle thereby increasing blood flow and tissue healing. The thoracic spine is that section of the spine that is below the neck and above the low back. It is also referred to as the mid back. It has multiple components that include: Vertebral Bodies: Boney building blocks that stack one upon another…
Read More About Prolotherapy For Thoracic PainProlotherapy Injections
It has been successful in the treatment of many disorders including neck, shoulder, knee, and ankle pain. Dr. Centeno recently published an article in The Journal of Prolotherapy in which he discusses the use of x-ray guidance with prolotherapy. This ensures that the injection is in the correct place to maximize clinical results. Dr. Centeno discusses the use of prolotherapy for the treatment of neck, knee, sacroiliac joint, ankle, ischial tuberosity, and shoulder pain. At the Centeno-Schultz Clinic x-ray guided prolotherapy is just one of the therapies utilized in the successful treatment of pain. Regenerative injection therapy (RIT) or prolotherapy…
Read More About Prolotherapy InjectionsPRP Injections
PRP is short for platelet-rich plasma, and it is autologous blood with concentrations of platelets above baseline values. The potential benefit of platelet-rich plasma has received considerable interest due to the appeal of a simple, safe, and minimally invasive method of applying growth factors. PRP treatments are a form of regenerative medicine that utilizes the blood healing factors to help the body repair itself by means of injecting PRP into the damaged tissue. In regenerative orthopedics, it is typically used for the treatment of muscle strains, tears, ligament and tendon tears, minor arthritis, and joint instability. There have been more than 30 randomized controlled trials of PRP…
Read More About PRP InjectionsThoracic Herniated Disc Surgery
Disc herniation is a painful medical condition in which the central portion of the disc is pushed outside of the disc and into the spinal canal. This occurs due to a weakness or injury to the outer sidewall of the disc. Pain, muscle spasm, muscle weakness, and numbness can occur. It can occur in the neck, low back, and thoracic spine. When conservative treatments fail, patients are often referred for thoracic herniated disc surgery. The goal of thoracic herniated disc surgery is to remove that portion of the herniated disc that is responsible for the ongoing pain and compression of the nerves.
Read More About Thoracic Herniated Disc SurgeryThoracic Spine Surgery
Thoracic spine surgery is a major surgery aimed at treating injuries in the thoracic spine. Because of the complex anatomy and close proximity to the heart and lungs, there are significant surgical risks and complications. Surgery on the thoracic spine can take hours and may require deflating the lung in order to gain access to the thoracic injury. Recovery can be lengthy depending upon the specific thoracic spine surgery performed. There are several different types of thoracic spine surgery. The specific thoracic spine performed depends upon the underlying thoracic injury and a symptoms of the patient. For example, a thoracic disc herniation…
Read More About Thoracic Spine SurgeryOur Doctors Who Treat Thoracic Outlet Syndrome
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate and PRP for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI).
Other Resources for TOS
-
Understanding the Thoracic and Lumbar Spines
The thoracic spine and lumbar spine make up a vital nexus of stability and mobility in the human body. In this exploration, we delve into the biomechanics and complexities that define these regions, unraveling their significance in posture, movement, and overall well-being. Understanding the thoracic and lumbar spine not only illustrates the mechanics of our…
-
Understanding the Role Of The Thoracic Spine Muscles
The thoracic spine plays a critical role in the stability and mobility of the upper body. Comprised of twelve vertebrae and an intricate network of muscles and ligaments, it serves as a central pillar supporting the structure and movement of the body. Understanding the role and function of thoracic spine muscles is pivotal for anyone…
-
Degenerative Changes Of The Thoracic Spine
Degenerative changes of the thoracic spine involve the gradual loss of normal structure and function over time. There are several different causes which are discussed in detail below. The thoracic spine is composed of many different and important components that are susceptible, both to injury and generalized wear and tear. The degeneration can occur in…
-
The Ultimate Guide To Thoracic Spine Exercises
Thoracic spine exercises are important for several reasons. First, they can help improve thoracic mobility, reducing the risk of spinal injuries and improving posture. Second, they can help to strengthen the muscles of the upper back and shoulders. Finally, thoracic spine exercises can help improve breathing mechanics. What Is Thoracic Spine? The thoracic spine, also…
-
Where Is The Thoracic Spine?
The thoracic spine is a region of the spine that is located in the middle back. It is located below the cervical spine and above the lumbar spine. It is composed of 12 vertebrae that are numbered T1-12. The T denotes the thoracic spine. It has many important functions which are discussed below. Location Of The…
-
Symptoms of Thoracic Herniated Disc
Your mid back pain has been unrelenting since the accident. Rest, medications, and physical therapy have failed to provide significant or sustained benefits. Your doctor thinks you have a thoracic disc herniation and thinks you have a thoracic herniated disc. What are the symptoms? And what can you do? Let’s dig in. What Is A…
References:
- Yuschak E, Haq F, Chase S. A Case of Venous Thoracic Outlet Syndrome: Primary Care Review of Physical Exam Provocative Tests and Osteopathic Manipulative Technique Considerations. Cureus. 2019;11(6):e4921.
- Ciampi P, Scotti C, Gerevini S, et al. Surgical treatment of thoracic outlet syndrome in young adults: single centre experience with minimum three-year follow-up. Int Orthop. 2011;35(8):1179-86.
- Teijink JAW, Pesser N, van Grinsven R, van Suijlekom H, van Sambeek MRHM, van Nuenen BFL. [Neurogenic thoracic outlet syndrome]. Ned Tijdschr Geneeskd. 2017;161:D1385.
- Moore R, Wei Lum Y. Venous thoracic outlet syndrome. Vasc Med. 2015;20(2):182-9.
- Köknel Talu G. Thoracic outlet syndrome. Agri. 2005;17(2):5-9.
- Lindgren KA. Conservative treatment of thoracic outlet syndrome: a 2-year follow-up. Arch Phys Med Rehabil. 1997;78(4):373-8.
- Novak CB, Collins ED, Mackinnon SE. Outcome following conservative management of thoracic outlet syndrome. J Hand Surg Am. 1995;20(4):542-8.
- Dobrusin R. An osteopathic approach to conservative management of thoracic outlet syndromes. J Am Osteopath Assoc. 1989;89(8):1046-50, 1053-7.
9.Brooke BS, Freischlag JA. Contemporary management of thoracic outlet syndrome. Curr Opin Cardiol. 2010;25(6):535–540. - Foley JM, Finlayson H, Travlos A. A review of thoracic outlet syndrome and the possible role of botulinum toxin in the treatment of this syndrome. Toxins (Basel). 2012;4(11):1223–1235.
- Finlayson HC, O’Connor RJ, Brasher PMA, Travlos A. Botulinum toxin injection for management of thoracic outlet syndrome: a double-blind, randomized, controlled trial. Pain. 2011;152(9):2023–2028.
- Hawkins AT, Schaumeier MJ, Smith AD, et al. Concurrent venography during first rib resection and scalenectomy for venous thoracic outlet syndrome is safe and efficient. J Vasc Surg Venous Lymphat Disord. 2015;3(3):290-4.
- Hosseinian MA, Loron AG, Soleimanifard Y. Evaluation of complications after surgical treatment of thoracic outlet syndrome. Korean J Thorac Cardiovasc Surg. 2017
- Jones MR, Prabhakar A, Viswanath O, et al. Thoracic Outlet Syndrome: A Comprehensive Review of Pathophysiology, Diagnosis, and Treatment. Pain Ther. 2019;8(1):5-18.