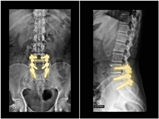
Transforaminal Lumbar Interbody Fusion (TLIF)
Risks, Complications, Success Rate, & Alternative Options
Am I CandidateIf you have been dealing with spine pain such as low back pain, neck pain, or nerve symptoms down the leg or arm and have failed all treatments – it is likely that your surgeon consultation went over the possibility of a Fusion! Most Fusion techniques are described as PLIF, TLIF, or ALIF. Acronyms for surgical approaches used for Fusion surgeries…..today let’s dig into one of the most common techniques, TLIF = “Transforaminal Lumbar Interbody Fusion.”
What Is the TLIF Technique
Transforaminal Lumbar Interbody Fusion is a variant of the Posterior Lumbar Interbody Fusion (PLIF) technique described by Cloward in the 1950s. PLIF has been associated with the high incidences of neurological complications, up to 13.6% of permanent neurologic lesions in Barnes’ et al. study, in particular of the traversing nerve root (2,3) This is due to the fact that a great amount of traction on the dural sac is required to implant the interbody fusion devices. Surgeons have transitioned to TLIF in efforts to reduce complication rates.
PLIF
PLIF = Posterior Lumbar Interbody Fusion. In this fusion technique, the vertebrae are reached through an incision in the patient’s back (posterior). PLIF is done with a 3-6 inch incision is made in the patient’s back. The spinal column is revealed after the muscles are retracted away. The surgeon then carefully removes the lamina (laminectomy) in addition to removing parts of the facet joint to get access to the nerve root and intervertebral disc. Then the surgeon removes the affected disc and surrounding tissue and prepares bone surfaces of adjacent vertebrae for fusion à Implants inserted. Once the disc space is prepared, a bone graft, allograft or BMP (bone morphogenic protein) with a cage, is inserted into the disc space to promote fusion between the vertebrae. Rods and Screws are then secured in place to add additional support
TLIF
Transforaminal Lumbar Interbody Fusion. This fusion surgery is a refinement of the PLIF procedure because PLIF leads to too many complications such as nerve injury. The TLIF technique involves approaching the spine in a similar manner as the PLIF approach but more from the side of the spinal canal through a midline incision in the patient’s back. This approach greatly reduces the amount of surgical muscle dissection and minimizes the nerve manipulation required to access the vertebrae, discs and nerves. The TLIF approach is the preferred method of interbody fusion as it is generally less traumatic to the spine, is safer for the nerves, and allows for minimal access and endoscopic techniques to be used for spinal fusion
ALIF
ALIF stands for Anterior Lumbar Interbody Fusion. This procedure is similar to PLIF, however, it is done from the front (anterior) of the body, usually through a 3-5 inch incision in the lower abdominal area or on the side. But this approach is infrequent due to the major blood vessels, bowels, and other critical organs they need to maneuver around to get access to the spine!
What Is the Successful Rate for TLIF
Success rates vary depending on what literature you read and recently all orthopedic surgery literature has come under fire for the lack of significant high-level studies showing long-term success rates. In recent years an orthopedic surgeon asked the question – what is the level of evidence currently for orthopedic surgeries? In 2015 a letter (5) to the editor of the British Medical Journal (BMJ) calling out the level of evidence in orthopedic literature concluded that 80% of all orthopedic surgeries have inadequate evidence to support their use! Last year, Dr. Buford continued the trend with a talk given at the recent Interventional OrthoBiologics Foundation and you can listen here. He showed that the current level of evidence being published by the top orthopedic surgery journals was a level 3 study = a case-control study, which are studies that are not blinded and not randomized.
Most recently the British Journal of Medicine published (6): “Common elective orthopaedic procedures and their clinical effectiveness: umbrella review of level 1 evidence.” One of the common orthopedic surgeries reviewed was Lumbar Fusion. A full review of the article was done by Dr. Centeno here. But in the end, the study concluded:
“no strong, high-quality evidence base shows that many commonly performed elective orthopaedic procedures are more effective than non-operative alternatives. Despite the lack of strong evidence, some of these procedures are still recommended by national guidelines in certain situations.”
Based on the current level of evidence we do not know the real success rates for Transforaminal Lumbar Interbody Fusions!
What Are the Risks and Complications Associated with the TLIF?
Despite not knowing the real success rate, these studies demonstrated that complication rates can be as high as 23% (4) with 325,000 procedures annually (7) =74,750 injured
These complications can be permanent debilitating injuries:
- Infection: Infection typically requires repeat operation and replacement of the instrumentation.
- Nerve Root Irritation: With traction placed on the spine, can lead to traction injuries and bone removal and lead to nerve injuries in addition, access to the disc requires nerve manipulation which can further injure the nerve roots!
- Nerve Damage from Pedicle Screws: If the surgeon takes a bad approach to the screw placements, they can impale the nerve root leading to weakness.
- Cage Anterior Migration: Occurs in patients affected by obesity.
- Blood loss
- Adjacent Segment Disease: Happens to ALL based on biomechanical properties when you fuse a level in the spine….don’t know what Adjacent Segment Disease is? See below!
What Is Adjacent Segment Disease?
The development of pathology at the mobile segment next to a Lumbar or Lumbosacral Spinal Fusion (Levels above and below the fusions) has been termed Adjacent Segment Disease. Meaning after a fusion, the levels above and below the fused levels absorb additional stress causing premature degeneration of these levels over time. Initially reported to occur rarely, it is now considered a potential late complication of spinal fusion that can necessitate further surgical intervention. To read more about Adjacent Segment Disease see here https://regenexx.com/blog/long-term-fusion-risk/#gref
What Are My Nonsurgical Options?
Lumbar fusions / Transforaminal Lumbar Interbody Fusion are indicated for multiple conditions such as; listhesis (slippage front to back of vertebrae), instability, herniated nucleus pulposus, stenosis, hypertrophic facet arthritis, scoliosis, and vertebral compression fracture. Before a fusion happens, patients must fail conservative treatments that consist of:
- Physical Therapy
- Medication Management (medications such as NSAIDS, Steroids, Opioid management, Neuropathic medications
- Interventional Pain Management Injections
- Corticosteroid Epidurals
- Can give short term relief but can have diminishing returns..to learn more go here: https://centenoschultz.com/less-relief-with-successive-epidural-steroid-injections/
- Facet Steroid Injections
- Medial Branch Blocks
- Radiofrequency Ablation
- Corticosteroid Epidurals
All these treatments are designed to give short-term relief but do not address the underlying conditions and help mask the symptoms, but even worse, these treatments may even advance degeneration! For example, Radiofrequency Ablation – burns the sensory nerves to the facet joints BUT that nerve also controls the nerve to the multifidi muscles that support and stabilize each segment of the spine ….so while the sensory nerve is burned, you won’t feel the pain from the joint, over time inhibiting the protecting muscles that support the joint means that over time the joint will increase the stress it has on it and further advance the arthritis!
Over the last 2 decades, the advent of ortho-biologics has changed the face or Orthopedic care! We were the first in the world to introduce the concept of using your body’s own platelets and bone marrow-derived cells to promote the healing of tissue! We pioneered a better option compared to traditional medicine above which can help address the underlying conditions such as Lithesis and instability in addition to treating Disc injuries, Facet Arthritis and helping to control the degenerative process to ultimately help you avoid the need for Transforaminal Lumbar Interbody Fusion and the complications that come with it! We termed this new approach to treating orthopedic conditions using your own body to help stop the degeneration “Interventional Orthopedics”
What Is Interventional Orthopedics?
Interventional Orthopedics is a whole new medical specialty that we created. With the discovery and use of regenerative medicine and ortho-biologics – we now have a bigger tool belt that necessitated a new approach to orthopedic medicine! Interventional Orthopedics is using advanced imaging guidance to target certain structures that are causing the pain and identifying and treating the underlying cause of the pain.
For example: with Facet Syndrome causing low back pain – the Facets are the pain generators BUT the underlying condition that is causing extra stress on the facets is instability / lithese. For the best outcomes, we not only treat the Facets but also treat the ligaments that control the stability! We call this treating the “Functional Spinal Unit.”
The Procedure is called Perc-FSU! It’s the trusted alternative to spinal fusion.
What is the Perc-FSU Procedure?
Conclusion
Transforaminal Lumbar Interbody Fusions are invasive procedures that come with a high complication rate and we don’t even know the true success rate thanks to limited research! A better option, when traditional medicine fails, is to address the underlying conditions with the healing agents from your own body using interventional orthopedic techniques. If you have been dealing with low back pain or a surgeon recommended a TLIF, then contact our clinic for a telemedicine evaluation or in-person evaluation so we can discuss if you are a candidate for our non-surgical back treatments!
Doctors that Provide Alternatives to Spinal Surgery

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…
Read more
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreMore Resources for Avoiding Back Surgery
-
Spinal Anterior Longitudinal Ligament Function
Have you had a neck injury or whiplash trauma? Do you have neck pain, especially when looking up, and you don’t know the cause? Then you may want to learn about the cervical anterior longitudinal ligament (ALL). Anatomy of the Anterior Longitudinal Ligament The ALL is a strong, wide ligament that runs along the front…
-
Effective Thoracic Herniated Disc Treatment Exercises You Can Do
A thoracic herniated disc occurs when the soft center of a spinal disc in the thoracic area of the spinal region ruptures. This condition can lead to symptoms such as pain, numbness, and weakness in the chest, back, and potentially radiating down the arms, legs or abdomen. Effective thoracic herniated disc treatment often involves a…
-
The L5 Vertebra: Everything You Need to Know
The spine, consisting of 33 individual bones called vertebrae, is divided into five major regions: cervical (neck), thoracic (upper back), lumbar (lower back), sacral (pelvic region), and coccygeal (tailbone). These vertebrae are separated by intervertebral discs, which act as cushions and allow for flexibility in movement. The lumbar spine, also known as the lower back,…
-
L5 S1 Or Lumbosacral Joint: What Is It And What Should You Be Wary Of?
The L5 S1 joint, or the lumbosacral joint, is a critical joint. It lies between the lumbar segment of the spine and the auricular processes of the sacrum. The L5-S1 joint plays a vital role in transmitting the weight of the body via the sacrum and ilium downwards. The weight is distributed to the femur…
-
9 Safe and Effective Ways to Crack Your Lower Back
“Cracking” the back is a safe and effective way to stretch the joints of the spine. This exercise also relieves pain and discomfort in the joints. You’ve probably done it just after waking up or at the end of a long day without really thinking about it. The Benefits Of Cracking Your Lower Back There…
References:
1. Mura PP, Costaglioli M, Piredda M, Caboni S, Casula S. TLIF for symptomatic disc degeneration: a retrospective study of 100 patients. Eur Spine J. 2011 May;20 Suppl 1(Suppl 1):S57-60. doi: 10.1007/s00586-011-1761-2. Epub 2011 Apr 2. PMID: 21461695; PMCID: PMC3087043.
2. Interbody, posterior, and combined lumbar fusions.
Fraser RD Spine (Phila Pa 1976). 1995 Dec 15; 20(24 Suppl):167S-177S.
3. Anterior/posterior lumbar fusion versus transforaminal lumbar interbody fusion: analysis of complications and predictive factors. Hee HT, Castro FP Jr, Majd ME, Holt RT, Myers L
J Spinal Disord. 2001 Dec; 14(6):533-40.
4. Reis RC, de Oliveira MF, Rotta JM, Botelho RV. Risk of complications in spine surgery: a prospective study. Open Orthop J. 2015 Jan 31;9:20-5. doi: 10.2174/1874325001509010020. PMID: 25674185; PMCID: PMC4321205.
5. Lohmander LS, Roos EM. The evidence base for orthopaedics and sports medicine. BMJ. 2015 Jan 2;350:g7835. doi: 10.1136/bmj.g7835. PMID: 25555826.
6. Common elective orthopaedic procedures and their clinical effectiveness: umbrella review of level 1 evidence BMJ 2021https://www.bmj.com/content/374/bmj.n1511
7. iData Research. How Many Spinal Fusions are Performed Each Year in the United States? https://idataresearch.com/how-many-instrumented-spinal-fusions-are-performed-each-year-in-the-united-states/ Accessed 7/21/21
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.