The Tenex Procedure
Minimally invasive technology used to treat chronic tendon and plantar fascia disease at its source.
Tenex Health TX® System Procedure: Everything You Need to Know
Are you suffering from chronic tendon or plantar fascia pain?
Tendinitis (or tendonitis) is a repetitive stress injury caused by use and overuse during activity resulting in the irritation or inflammation of the tendon. Even the most mundane of repetitive motions can create microtears in the tendon which can lead to chronic tendinopathy (tendon degeneration) when those tears do not heal properly. In some cases, this may cause the formation of calcification within the tendon, further increasing pain, resulting in plantar fasciitis or other tendon degenerative diseases.
Are you suffering from pain caused by a bone spur?
A bone spur, also known as an osteophyte or enthesophyte, is a bony formation that develops on normal bone, and these growths can press against, rub on, and eventually cause inflammation, wear and tear, and pain of the surrounding tissues. If a bone spur is the source of your pain, restricting use may help reduce symptoms, but the symptoms will usually return.

If you answered yes to either of these questions, you may be a candidate for a Tenex treatment.
The Tenex Health TX® System is a minimally-invasive, percutaneous procedure using ultrasonic energy to treat pain-generating soft and hard tissue conditions. This treatment is clinically proven to remove tendon pain for over 85% of patients1,2,3,4,5. If conservative approaches such as physical therapy, cortisone injections, medication, and downtime do not provide relief, Tenex may be your next option.
Using this technique, we help patients restore musculoskeletal function, may provide quick pain relief, and avoid invasive surgery and dangerous drugs. Tenex may also be effective if you have had a failed surgical procedure.
Patient benefits may include:
- Rapid pain relief
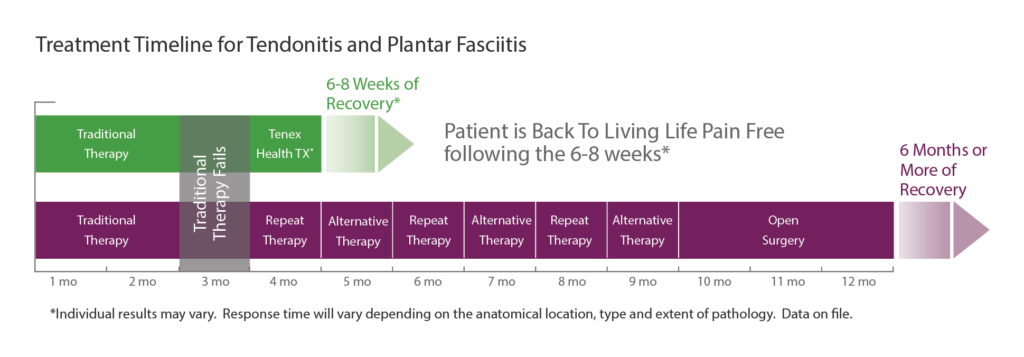
- Quick recovery and return to normal activities in 6-8 weeks (compared to 6 months or more with an open surgical procedure)
- Single treatment
- Typically performed with local anesthetic (no general anesthesia)
- No sutures (requires only a small, adhesive bandage)
- Well-tolerated procedure
- Does not disturb surrounding healthy tendon
- Stimulates the body’s healing response in the tendon
*individual results may vary
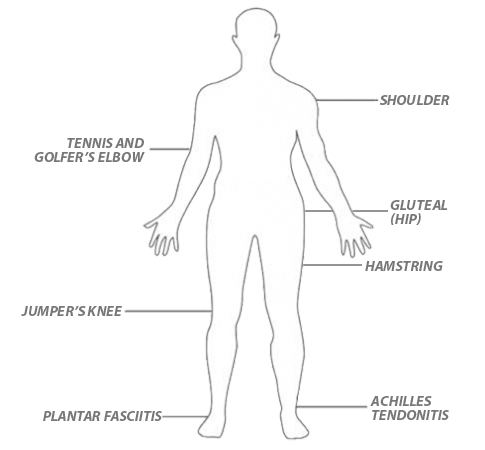
What areas of the body can Tenex Health TX treat?
Speak with us today if you are suffering from:
- Shoulder tendinitis (rotator cuff or biceps)
- Lateral or medial epicondylitis (tennis or golfer’s elbow)
- Gluteal tendinitis (hip)
- Pelvic hamstring tendinitis
- Patella tendinitis (runner or jumper’s knee)
- Achilles tendinitis (ankle)
- Plantar fasciitis (foot or heel)
- Calcific deposit in the tendon
- Pain associated with a bone spur or bony prominence
How does Tenex Health TX work?
Achilles Tendonitis
Heel pain is one of those issues that can affect most of what you do in a day and can be disabling. A common cause of heel pain is the Achilles tendon. What is the Achilles tendon? What is Achilles tendonitis? What are the different injuries? Is stem cell therapy for Achilles tendonitis a viable option? Where & What Is the Achilles Tendon? A tendon is a thick fibrous band of connective tissue that connects a muscle to bone. There are more than 30 million tendon and ligament injuries annually. The Achilles tendon, which is the thickest tendon in the body connects the calf muscles to the heel bone. It consists of the gastrocnemius and soleus muscles that unite to form a thick band that is immediately above the heel tab on your shoe. It enables the downward movement of the foot and bending of the knee.
Read More About Achilles TendonitisBone Spurs In The Knee
Bone spurs, also known as osteophytes, are abnormal growths that can form along any bony surface in the body. They most frequently occur where tendons and ligaments attach to the bone. As a result, they are more commonly seen in large mobile joints that support weight, such as the hips, spine, ankles, or knees. Surprisingly, most bone spurs are relatively benign but are a clinical sign of instability in the area. Research demonstrates that if a ligament has laxity, the constant strain at the insertion into the bone will elevate the surface of the bone, creating additional bone formation – this is known as a traction osteophyte.
Read More About Bone Spurs In The KneeCalcific Tendonitis
Calcific tendonitis, also known as calcifying tendonitis, is a condition characterized by the formation of calcium deposits in a tendon, most commonly in the rotator cuff tendons of the shoulder. These deposits are not due to injury or trauma but rather occur spontaneously. Tendons, the thick connective tissues that link muscles to bones, aren’t usually calcified. However, in calcific tendonitis, calcium builds up in these tissues, which can result in inflammation and severe pain. This condition tends to occur more commonly in adults between 30 and 60 years old, and it’s more prevalent in women than in men.
Read More About Calcific TendonitisGluteal Tendinopathy
Tendinopathy is a group of tendon disorders. The most common form of Tendinopathy is Tendinosis (1). Tendinosis is a degenerative condition that is characterized by collagen degeneration and micro-trauma in the tendon due to repetitive overloading. Gluteal Tendinopathy is a clinical condition in which there is moderate to severe debilitating pain due to injury of the Gluteal tendons. It is the most common Tendinopathy in the lower leg (2) and is more common in women (3). In most cases, physical examination alone is sufficient to diagnose Gluteal Tendinopathy. If symptoms continue despite conservative care, other studies may be warranted which include ultrasound and MRI.
Read More About Gluteal TendinopathyGolfer’s Elbow
Golfer’s elbow involves tears in the ulnar collateral ligament and pain or soreness on the inside of the elbow. The bony bump you feel there is the medial epicondyle of the humerus (upper arm bone). There are five forearm muscles that attach at this point, all of which are involved in helping to flex or rotate the forearm and wrist. Pain can get worse when you throw a ball, grip a dumbbell, turn a screwdriver, and other movements that involve the fingers, hand, wrist, and/or elbow. Tennis elbow is similar, however, it refers to the outside of the elbow, at the lateral epicondyle.
Read More About Golfer’s ElbowHamstrings Tendinopathy
Hamstring tendinopathy, a condition that causes pain and tenderness in the hamstring tendons, represents a common but often misunderstood musculoskeletal issue. It typically occurs in athletes and individuals engaged in high-intensity activities but isn’t limited to them. This condition, including its more specific form, high hamstring tendinopathy, can significantly impact daily and athletic performance, making understanding its nuances critical.
Read More About Hamstrings TendinopathyPatellar Tendonitis
What is the Patellar Tendon? A tendon is a piece of connective tissue that connects muscle to bone. It serves to move the bone or a given joint. The patellar tendon is a major tendon in the knee. It is located at the bottom of the kneecap (patella) and stretches down to the shin. The patellar tendon enables you to extend your knee, kick, run, and jump. What is Patellar Tendinitis? Patellar tendinitis is an irritation and inflammation of the tendon that connects your kneecap (patella) to your shinbone. Patellar tendinitis, also known as jumper’s knee, can affect anyone. The most common symptom is pain at the shin or lowest part of the kneecap…
Read More About Patellar TendonitisPatellar Tendonitis Or “Jumper’s Knee”
Patellar tendonitis, or jumper’s knee, occurs due to small tears in the patellar tendon. It is commonly seen in individuals who frequently jump – hence the name – but can also occur in running sports or sports that require rapid changes of direction. Jumper’s knee is a condition that is frequently observed in the athlete population, but has a very good prognosis provided it is diagnosed and treated correctly. This post covers the symptoms, diagnostic tests, and treatment options for patellar tendonitis.
Read More About Patellar Tendonitis Or “Jumper’s Knee”Plantar Fasciitis
Your heel pain initially was mild and aching. It is now a constant forest fire at the base of your heel. Each morning you take your first step with great trepidation knowing that the searing pain is literally a step away. Medications, rest, and physical therapy have not helped. Your doctor is concerned and thinks you may have Plantar Fasciitis. What is Plantar Fasciitis? What are the symptoms of Plantar Fasciitis? What are the risk factors? Is Plantar Fasciitis simply inflammation? What are the treatment options for Plantar Fasciitis? What to do for Plantar Fasciitis so bad I can’t walk? Beware as not all heel pain is Plantar Fasciitis.
Read More About Plantar FasciitisPrecisely targets your damaged tissue.
Your doctor will use image-guidance to identify and target the exact location of your injury (damaged tendon tissue, bone spur, and/or calcific deposit).
Removes the damaged tissue.
Following the identification of the pain generator, the area is numbed using a local anesthetic. After being numbed (which is comparable to a bee sting), many people say that during the procedure, they only felt a slight pressure (if anything at all). Your doctor then uses ultrasonic energy, applied with the TX MicroTip, designed to safely break down and remove the damaged tissue. This requires only a small incision into the target, diseased tissue, and it is effective for the elimination of degenerative tissue, leaving healthy tendons unharmed.
Requires no stitches.
After the procedure, your doctor will apply only a small adhesive bandage. Though you will likely be awake during the procedure (depending on what, if any, additional Centeno-Schultz procedures you receive on the same day), our safety protocols most likely require you have someone to drive you home afterward.
May offer rapid pain relief and faster recovery.
Following a Tenex Health TX procedure, many people are back to normal activity within 6-8 weeks and even less in some cases. The minimally invasive approach and targeted removal of the tissue mean there is less discomfort and minimal downtime when compared with open surgery. Your recovery timeline depends on the location and extent of the damaged tissue being treated.
VIDEO: Watch how your doctor uses Tenex Health TX to treat chronic tendon and plantar fascia pain:
The medical procedure called percutaneous tenotomy or percutaneous fasciotomy using the Tenex procedure is specifically designed for those suffering from painful conditions associated with chronic tendon or plantar fascia damage. It is also known as chronic tendinosis/plantar fasciosis or tendinopathy/plantar fasciopathy. For more information, visit www.tenexhealth.com.
Clinical References:
- Freed L, Ellis M, Johnson K, Haddon T. Fasciotomy and surgical tenotomy for chronic Achilles insertional tendinopathy: a retrospective study using ultrasound-guided percutaneous microresection. J Am Podiatr Med Assoc. 2019; 109(1):1-8.
- Koh JS, Mohan PC, Howe TS, Lee BP, Chia SL, Yang Z, Morrey BF. Fasciotomy and surgical tenotomy for chronic lateral elbow tendinopathy: early clinical experience with a novel device for minimally invasive percutaneous microresection. Am J Sports Med. 2013; 41(3):636-644.
- Patel M. A novel treatment method for refractory plantar fasciitis. Am J Orthop. 2015;44(3):107-110.
- Razdan R, Vanderwoude E, Braun A, Morrey BF. Percutaneous ultrasonic fasciotomy: a novel approach to treat chronic plantar fasciitis. J Surg Proced Tech. 2018;3(102):1-6.
- Seng C, Mohan PC, Koh SB, Howe TS, Lim YG, Lee BP, Morrey BF. Ultrasonic percutaneous tenotomy for recalcitrant lateral elbow tendinopathy: sustainability and sonographic progression at 3 years. Am J Sports Med. 2016; 44(2):504-510. (epublished: Nov 2015).
MKT-111 REV E
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.