Nowadays, more and more people are dealing with neck pain and headaches. There are a lot of different causes of neck pain and headaches, one of which is intracranial hypertension. Anyone diagnosed with intracranial hypertension will want to know more about it.
For example, you might wonder why it causes headaches or if the condition is caused by something else, like internal jugular vein (IJV) compression. You’ll probably also be wondering whether neck problems can make it worse, or whether you’ll need surgery to take care of it.
The following guide will answer the common questions about intracranial hypertension – along with everything you need to know about the condition and how you can treat it.
What Is Intracranial Hypertension?
Intracranial hypertension is a neurological disorder characterized by increased pressure in the cranial or brain cavities. As a result, an abnormal amount of blood or cerebrospinal fluid (CSF) builds up around the brain and spinal cord, leading to neck pain and headaches.
It’s also worth mentioning that IJV compression can sometimes lead to intracranial hypertension, as well as cause similar symptoms such as headaches and neck pain on its own.
What Is The Internal Jugular Vein?
The IJV is one of the three major veins (along with the exterior and anterior veins) in the neck responsible for transporting blood back to the heart from the head and neck area. It’s located in the carotid sheath, which also contains the internal carotid artery and the vagus nerve.
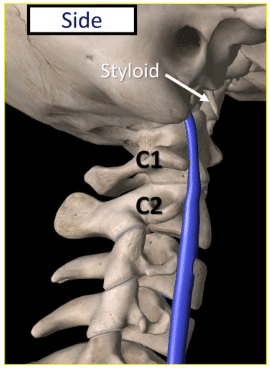
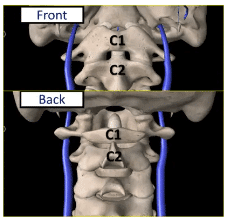
The blood travels through the vein in front of the upper cervical spine (as indicated above), right in front of the transverse process (TP) of C1.
The TP is a small bony projection on each side of the vertebrae (represented by the side projection protruding from C1, located right behind the vein as you can see in the diagrams above).
The proximity between the IJV (in blue) and the C1 vertebra is indicated in the front and back diagrams above. Notice how close the IJV is to the TP.
Internal Jugular Vein Compression And CCI
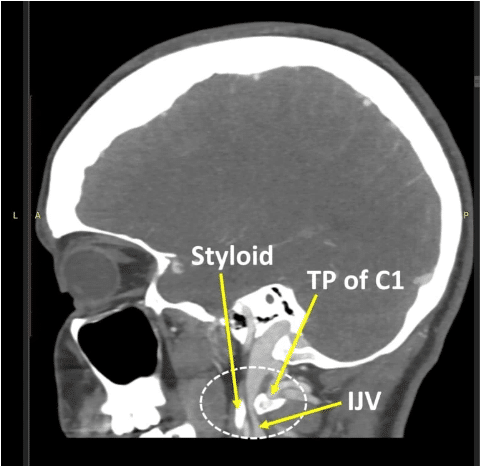
In the CT venogram above, you can see how the internal jugular vein can become compressed between the TP of C1 and the styloid, which is the bone that projects from the bottom of the skull. In addition, the styloid can look longer when captured on X-ray because the ligaments that attach to it can become calcified.
Can Craniocervical Instability (CCI) Compress The Internal Jugular Vein?
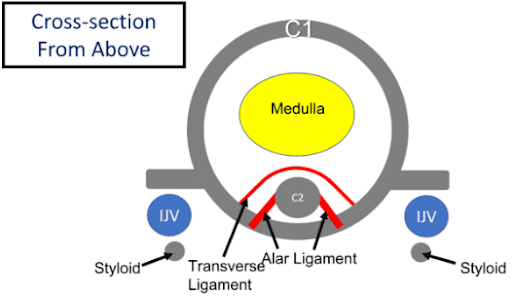
Craniocervical Instability, or “CCI,” occurs when the upper neck ligaments (which connect between the skull and the upper cervical spine) become loose, resulting in instability. As you can see in the image above, the small projections from the side of the C1 vertebra are right behind the IJV.
The IJV is being compressed between the TPs of the C1 vertebra and the styloids. The transverse and alar ligaments (pictured in red) hold the C1 vertebra to the dens of the C2 vertebra.
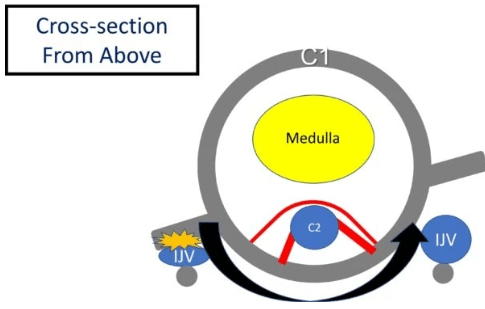
Here, we see what happens when the transverse and alar ligaments become loose. As you see, the C1 vertebra shifts forward, thereby causing internal jugular vein compression. Internal jugular vein compression can also occur more on one side if the C1 is abnormally rotated due to loose ligaments.
The same thing can also happen more on one side if C1 is rotated abnormally due to lax ligaments.
What Are The Symptoms Of Internal Jugular Vein Compression And Intracranial Hypertension?
There are a lot of different symptoms that patients may experience from IJV compression and intracranial hypertension, to the point where there are a lot of opinions regarding what the primary symptoms actually are.
However, a study measuring the reported symptoms of IJV compression indicates that the top three symptoms patients complained about were insomnia, tinnitus (ringing in the ears), and head noises (such as whooshing sounds). The fourth most reported symptom was hearing problems.
Interestingly, neck pain and headaches were the least commonly reported – despite those being the two symptoms our CCI patients tend to believe are the result of IJV compression.
Diagnostic Testing To Rule Out Internal Jugular Vein Compression
If you have intracranial hypertension, you’d naturally be worried that it’s being caused by IJV compression. Unfortunately, identifying IJV as the root cause of symptoms like neck pain and headaches can be complicated.
This is because there is no diagnostic test specifically designed for this problem, which means there is no way to identify the underlying cause of the symptoms with 100% accuracy.
To demonstrate this issue, let’s examine an example. Let’s say a patient complains that they are suffering from headaches that they believe originate from their upper neck. A magnetic resonance imaging (MRI) test shows that the C0-C1 facet joint is swollen and arthritic. Research indicates that when this joint hurts, pain signals are sent to the head.
To officially diagnose the affected joint, doctors would perform a diagnostic numbing injection under x-ray guidance using radiographic contrast. If the headache disappears once the C0-C1 joint is numbed, we can reasonably assume the headache pain is being caused by that joint.
However, if it doesn’t go away, the headaches are likely coming from somewhere else. This diagnostic test is called a “confirmatory block.” Essentially, we can numb any structure, confirming if it’s causing the painful symptom or not.
So then, what’s the problem? The problem is that this can’t be done for IJV compression. If we believe that the IJV is causing the patient’s headaches, there’s no way to use diagnostic imaging to perform a confirmatory block.
We would have to treat the IJV compression using an invasive procedure to see if the headaches disappear. The only thing we can definitely do is use diagnostic testing to determine if there is IJV compression. Only once we treat it will we find out if it’s what was causing the symptoms.
Keeping this in mind, the following are the diagnostic tests that can be performed to determine if a patient has IJV compression:
CTA Or CTV
Both computed tomography venograms (CTVs) and CT angiograms (CTAs) can be used to diagnose IJV compression, although CTV is considered to be the gold standard because it tends to be used more to study the veins, whereas a CTA is used more to study the arteries.
Both tests use radiographic contrast to take 3D pictures of the bones using CT scans. Both tests can be done whether the patient has their head and neck in a neutral position or turned.
MRI And Ultrasound
An MR angiogram (MRA) is a specialized MRI that can be used to diagnose IJV compression. However, it’s not as accurate as a CTV due to its longer imaging times and poorer imaging quality of the bones. Ultrasound imaging is another option, but it’s highly operator-dependent. If the ultrasound probe is off just a bit, it can result in the collection of inaccurate data about the IJV.
IJV Compression Treatment
If a patient is diagnosed with IJV using one of the previous diagnostic imaging tests, there are two primary ways to treat it. We can stabilize the CCI, or we can open up the IJV. The following is a brief overview of each treatment option:
Stabilize The CCI
If it’s determined that CCI is the cause of the IJV compression, then stabilizing the CCI is the best option. Although this can be done using a surgical fusion procedure, doing so is risky as it can result in potentially life-changing complications.
Fortunately, there are less invasive treatment options available these days. At Centeno-Schultz, our experienced clinicians inject a concentrate of your own bone marrow into the damaged and loose ligaments, causing them to tighten up.
Open Up The IJV
If IJV compression is diagnosed, one treatment option is to open up the IJV to reduce the pressure on it. There are a few ways that this can be done. One way is to surgically remove the styloid with or without shaving down the front of the C1 TP. The other way is to place a stent to open up the IJV.
However, these procedures don’t make much sense if CCI is causing the compression. Both options to open up the IJV are big procedures.
Both the styloid and the TP of C1 are important to neck stability, which means surgically removing any of these structures can cause more neck instability — which isn’t great if the patient has CCI, which is already causing neck instability. Stenting the IJV, in this case, won’t work either since the vein will continue to collapse under pressure.
Is IJV Compression Causing Your Symptoms?
If you have intracranial hypertension and it’s causing neck pain and headaches, then there are ways (as previously mentioned) to diagnose the root cause as IJV compression. However, it’s worth mentioning that you can have IJV compression and not have intracranial hypertension.
Unfortunately, IJV compression can be difficult to diagnose if you’re not experiencing any symptoms. This may not seem like an issue, since you would think that anyone with IJV compression would have symptoms as a result. However, it turns out that this is not the case.
Researchers recently conducted a study to determine how often patients with IJV compression experienced no symptoms at all. These researchers went through past CTA studies from patients who were mostly being worked up for carotid artery stenosis.
If IJV compression had been diagnosed in these particular patients, it would have been incidental. Basically, the IJV compression diagnosis was random and not linked to any symptoms typically caused by IJV compression.
Of those CTA studies, countless incidental diagnoses were made of IJV compression without any symptoms being linked. The following is a breakdown of the data:
- Moderate stenosis was identified in 33% of the right internal jugular vein and 25.9 percent of the left internal jugular vein.
- Severe stenosis was discovered in 24.1% of the right internal jugular vein and 18.5 percent of the left internal jugular vein.
- Severe bilateral extrinsic compression was identified in 9.3% of the cases.
- The styloid process and the posterior belly of the digastric muscle were found to be the most common causes of extrinsic compression.
The question you’re likely asking is how can all of these patients who were found to have IJV compression not have had any symptoms? The answer is “collateralization.”
What Is Collateralization?
Looking at the diagram above, you can see that there are several venous routes out of the brain. If one of these venous routes is blocked, the body will enlarge another to compensate. This is known as “collateralization.” Additionally, if a venous route is blocked, the body can also grow new veins around the compressed area. This is known as “collateralization.”
Essentially, collateralization is a process in which the body creates an alternate route for your blood flow to reach the brain if a vein is blocked or damaged.
Now the question is, if your headaches aren’t being caused by IJV compression or intracranial hypertension, then what is causing them? The thing is, there’s a laundry list of neck structures that can cause headaches if they are damaged or irritated, including:
- C0-C1 facet joint
- C1-C2 facet joint
- C2-C3 facet joint
- Greater occipital nerve
- Lesser occipital nerve
- Third occipital nerve at C2-C3
- Third occipital nerve at posterior C2
- Superficial cervical plexus at the SCM
- Supraorbital nerve
- Supratrochlear nerve
- Auriculotemporal nerve
- C2 dorsal root ganglion
- C2-C3 intervertebral disc
- Sphenopalatine ganglion
- Many muscle trigger points
Putting It All Together
If you have CCI and believe you might have IJV compression, then treatments to stabilize your upper neck is the first step you’ll need to take before considering invasive surgery. Additionally, even if you have diagnostic images indicating IJV compression, you can’t assume that this is the underlying cause of the symptoms you’re experiencing.
As such, you need to be cautious about deciding to get surgery as a result of an imaging test – especially since surgical procedures can lead to a wide range of complications. Ideally, surgery should be an absolute last resort. Instead, always choose the least invasive treatment to avoid unnecessary risks.
At the end of the day, IJV compression could be the underlying cause of intracranial hypertension – but it could also be a range of other conditions. Like any accurate diagnosis, a comprehensive diagnosis of your condition requires much more than just a diagnostic imaging test.
It’s like putting the pieces of a puzzle together – diagnosis involves a detailed analysis of the symptoms, a hands-on physical examination, various diagnostic tests, and the analysis of your response to treatment. A diagnostic imaging test is meaningless unless viewed in the context of a bigger picture.
Finally, even if it’s determined that IJV compression is the cause of your headaches and neck pain, it makes more sense to fix the CCI first.