Herniated Cervical Disc
In the United States, neck and back pain are major causes of disability, affecting millions of individuals each year.
According to the National Institute of Neurological Disorders and Stroke, back pain is the second highest leading cause of disability among adults in the United States, and neck pain is also a significant contributor to disability. Many instances of suffering from neck and back pain are due to herniated cervical discs.
So today, let’s dive into understanding the details of what a cervical disc herniation is and what can be done about it!
An Overview Of The Cervical Disc
Cervical discs, also known as intervertebral discs of the cervical spine, are the specialized structures located between the vertebrae in the neck region. These discs play a crucial role in providing cushioning, flexibility, and support to the cervical spine.
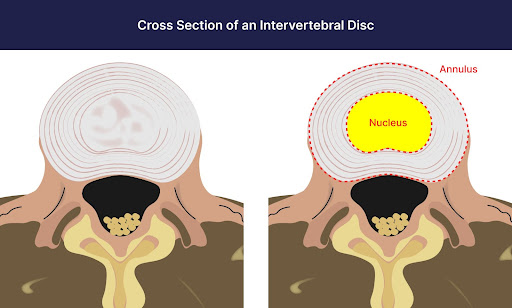
Structure: Cervical discs have a unique structure consisting of two main components:
- Nucleus Pulposus: The nucleus pulposus is the central, gel-like core of the disc. It is composed of a jelly-like substance with a high water content, giving it a soft and elastic nature. The nucleus pulposus is responsible for absorbing and distributing forces acting on the spine during movements, acting as a shock absorber.
- Annulus fibrosus: Surrounding the nucleus pulposus is the annulus fibrosus, which is a tough, fibrous ring-like structure made up of concentric layers of collagen fibers. The annulus fibrosus provides strength and stability to the disc and helps to contain the nucleus pulposus within the disc space.
Functions: The cervical discs perform several important functions:
- Shock absorption: The discs absorb and distribute forces acting on the cervical spine, reducing the impact on the vertebrae during movements such as walking, running, or jumping.
- Flexibility and movement: The discs allow for flexibility and mobility of the cervical spine, enabling a range of movements like bending forward, backward, and sideways, as well as rotational movements.
- Load-bearing: Cervical discs support the weight of the head and upper body, helping to maintain proper alignment and balance of the cervical spine.
- Spinal stability: The discs contribute to the overall stability of the cervical spine, working in conjunction with ligaments, muscles, and other spinal structures.
For more details visit here: this page
What Is A Cervical Herniated Disc?
Cervical discs can be subject to degeneration, injury, or conditions that affect their normal structure and function.
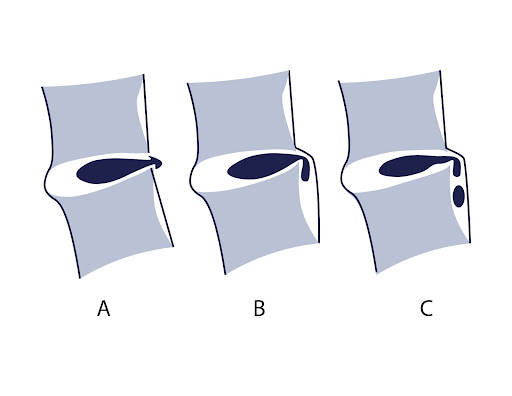
The structural component of a disc is the annulus; damage to this will allow the common cervical disc disorders:
- Herniated disc: When the annulus fibrosus weakens or ruptures, the nucleus pulposus can protrude outwards, pressing on nearby nerves and causing symptoms such as pain, numbness, and weakness.
- Degenerative disc disease: With age, the discs can undergo degenerative changes, including loss of water content, thinning, and deterioration, which can lead to pain and reduced mobility.
- Disc bulge: A disc bulge occurs when the annulus fibrosus protrudes beyond its normal boundaries, potentially compressing nearby structures.
Types Of Cervical Herniated Disc
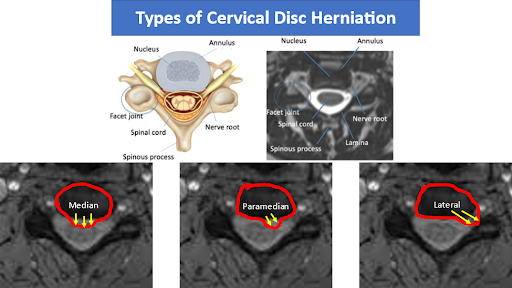
Cervical disc herniation refers to the displacement or protrusion of the intervertebral disc in the cervical spine, which can potentially compress the spinal cord or spinal nerves. Cervical disc herniations can be categorized into three main types based on their location: median, paramedian, and lateral herniations.
- Median herniation: A median herniation occurs when the disc protrudes centrally and compresses the spinal cord directly. It typically affects the structures in the midline of the spinal canal.
Median herniations may cause symptoms such as pain, weakness, numbness, or loss of sensation in both arms and legs. This type of herniation is less common in the cervical spine compared to the lumbar spine.
- Paramedian herniation: A paramedian herniation happens when the disc protrudes to one side of the spinal canal. It often leads to compression of the adjacent spinal nerve roots rather than the spinal cord itself.
Depending on the specific location of the herniation, it may cause symptoms on one side of the body, including neck pain, radiating arm pain, muscle weakness, and sensory changes in the corresponding dermatomal distribution.
- Lateral herniation: A lateral herniation occurs when the disc protrudes to the side of the intervertebral foramen, where the spinal nerves exit the spinal canal. This type of herniation primarily affects the exiting nerve roots.
Lateral herniations commonly cause symptoms such as sharp or shooting arm pain, numbness, tingling, and muscle weakness in the corresponding nerve distribution. Lateral herniations can also compress the nerve roots within the neural foramen.
Symptoms Of Cervical Herniated Disc
It is important to note that cervical disc herniations can vary in severity, and the specific symptoms and their intensity can depend on factors such as the extent of disc protrusion, the degree of nerve compression, and individual variations.
Treatment options for cervical disc herniations may include conservative measures like rest, pain medication, physical therapy, and in some cases, surgical intervention to relieve compression and restore normal function. The choice of treatment depends on the individual’s symptoms, severity of herniation, and response to conservative measures.
Cervical disc herniations can manifest with various symptoms depending on the location and extent of the herniation. Here is a description of the symptoms commonly associated with cervical disc herniations:
- Cervicogenic headache: Cervicogenic headaches are headaches that originate from the cervical spine. Cervical disc herniations can cause referred pain to the head, resulting in headaches that are typically localized to the base of the skull or radiate to the forehead or temples.
- Tingling or numbness in arms or hands: Cervical disc herniations that compress spinal nerves can lead to tingling sensations (paresthesia) or numbness in the arms, hands, and fingers. The affected nerve’s specific distribution determines the area where the tingling or numbness is felt.
- Weakness in arms/hands: Compression of spinal nerves due to cervical disc herniation can result in muscle weakness in the arms and hands. The weakness may vary in severity and can affect grip strength, fine motor skills, and coordination.
- Reduced neck mobility: Cervical disc herniations may limit the normal range of motion in the neck. Individuals may experience stiffness, difficulty turning the head, and restricted neck movement due to pain or mechanical obstruction caused by the herniated disc.
- Base of skull headaches: In addition to cervicogenic headaches, cervical disc herniations can also cause headaches specifically localized to the base of the skull. These headaches may be associated with neck pain and restricted neck movement.
- Radiating pain with movement: Movement of the neck, such as bending forward or turning, may exacerbate pain in individuals with cervical disc herniations. The pain may radiate from the neck to the shoulders, arms, and even down to the hands.
- Pain aggravated by coughing, sneezing, or laughing: Activities that increase intra-abdominal pressure, such as coughing, sneezing, or laughing, can intensify the pain experienced with cervical disc herniations. This is due to increased pressure on the already compressed nerves.
- Difficulty with fine motor tasks: Cervical disc herniations affecting nerve function can lead to difficulties with fine motor tasks requiring dexterity and coordination in the hands, such as writing, buttoning clothes, or handling small objects.
- Loss of coordination or balance in severe cases: In more severe cases of cervical disc herniation, compression of the spinal cord or significant nerve involvement can lead to neurological defects. These defects may include a loss of coordination, balance issues, and difficulty walking.
- Cervicalgia: Cervicalgia is also known as neck pain, which is an all-too-common, unpleasant pain. Cervicalgia is also known as neck pain, which is an all-too-common, unpleasant pain.
- Neck Muscle Spasms: Neck spasms are an involuntary tightening of muscles in the neck. They can be abrupt in onset and gradually increase after a given activity. Typically they involve the entire neck but maybe more intense on one side leading to an involuntary rotation of the neck.
Deep Dive Into Symptoms
Arm Pain at Night
Arm pain at night can be miserable. The pain can interrupt your sleep and erode your quality of life. Irritability becomes increasingly more common. What are the causes? When should I worry about it? What are the treatment options for arm pain at night? The neck is composed of 7 boney building blocks numbered 1- 7. Sandwiched between the bones is a disc that functions as an important shock absorber. The cervical discs are susceptible to injury due to trauma, degeneration, repetitive motion, and surgery. Common disc injuries include disc bulges, and herniations. The injured disc can compress or irritate one or more nerves resulting in arm pain at night. It can…
Read More About Arm Pain at NightArm Throbbing
In many patients, irritated neck nerves don’t present as a symptom in the neck. In fact, sometimes the only symptoms of irritated nerves in the neck occur in the arm muscles, as either tightness, throbbing, or both. While the arm throbbing might be frustrating as it’s happening, you might not think a whole lot about it, especially if it only happens on occasion. However, ignoring it is not a good idea since it is often a warning signal of a bigger problem in the neck. These body connections occur all the way back to when we were a fetus, like the neck, shoulder, and arm.
Read More About Arm ThrobbingCervicalgia / Neck Pain
Cervicalgia is also known as neck pain, which is an all-too-common, unpleasant pain. Read here to learn the symptoms, diagnosis, and treatment options. We will discuss other causes for cervicalgia. What symptoms are associated with cervicalgia? How is cervicalgia diagnosed? What are the treatment options for cervicalgia? Cervicalgia is a medical term used to describe neck pain. It is very common and affects approximately 2/3 of the population at some point in their life. Cervicalgia is the 4th major cause of disability. Risk factors include injury, prior history of neck and musculoskeletal pain, jobs that require a lot of desk work, low social support, job insecurity, physical weakness, and poor computer station setup.
Read More About Cervicalgia / Neck PainChronic Headaches
Do you suffer from chronic headaches? Maybe it’s a daily issue, maybe once a week, maybe even less often, but one thing’s for sure—when a chronic headache kicks in, it can be a real pain in the neck, literally. In order to effectively address chronic headaches, you have to first determine if the pain is caused by a problem in your neck. Let’s take a look at a few neck issues that can cause headaches: Weak neck muscles – The head, on average, weighs about ten pounds, so when the neck muscles are weak, it can make your head feel a bit like a bowling ball that your neck can’t quite balance. There are many muscles that, along with the cervical spine, work together to help support the neck and aid movement…
Read More About Chronic HeadachesFeeling Of Pins And Needles In Fingers
Are you experiencing the sensation of pins and needles in your fingertips? This is a common symptom of cervical radiculopathy. Although many conditions can cause pins and needles, if it is accompanied by neck pain, then cervical radiculopathy would be at the top of the diagnostic list. Cervical radiculopathy also referred to as a “pinched nerve.” is a medical syndrome that occurs when a nerve root in the neck ( cervical spine) becomes compressed or irritated leading to symptoms that include pain, numbness, tingling, and potentially weakness. It occurs in about 85 people per 100,000 (1). Read this post to find out more about cervical radiculopathy and how it can cause pins and needles in your fingertips.
Read More About Feeling Of Pins And Needles In FingersLeft Arm Numbness
Treatment depends upon the underlying cause of the arm numbness. Left-arm numbness is a warning sign that requires attention. As noted above unexplained numbness requires immediate attention. At the Centeno-Schultz Clinic, we are experts in the treatment of left-arm numbness due to cervical nerve irritation, cervical stenosis, thoracic outlet syndrome, and peripheral nerve injuries. When appropriate first-line treatment should involve conservative care including physical therapy and stretching. Steroid injections should be avoided as they are toxic to orthopedic tissue and can accelerate damage. Surgery for Cervical Stenosis and Thoracic…
Read More About Left Arm NumbnessMotor Issues
Cervical radiculopathy is a condition caused by compression of a cervical nerve root, which can result in pain and sensorimotor deficits. Nerve roots are mixed nerves which are responsible for sensory and motor function. There are eight cervical nerve roots that branch off from the spinal cord, labeled from C1-C8. Each cervical nerve root supplies a particular region of skin, called a dermatome,and innervates certain groups of muscles, called a myotome. When the cervical nerve root is compressed, the sensory supply to the dermatome in the upper limb can be altered. This can lead to pain, decreased sensation, the feeling of pins and needles, and even numbness. This can also coincide with muscle weakness, and a decreased reflex response.
Read More About Motor IssuesMuscle Spasm In Shoulder
A muscle spasm, also known as a muscle cramp, is a sudden and involuntary contraction or tightening of a muscle or group of muscles. This can occur in any part of the body but is most commonly experienced in the legs, arms, and back. These spasms can last for a few seconds up to many minutes. Occasional muscle spasms may not be something to worry about, but chronic muscle spasms can be a serious issue. In the shoulder, there are many muscles that can go into spasm. These spasms or cramps can cause pain, stiffness, and limited mobility.
Read More About Muscle Spasm In ShoulderPain At The Base Of The Neck
Pain at the base of the neck is the fourth most common cause of disability. It is important to understand the cause of the pain because it determines what treatment you need. While most pain at the base of the neck resolves without treatment, 50% of patients tend to have lingering symptoms and need to address the specific cause.
Read More About Pain At The Base Of The NeckPain In The Left Side Of The Neck
Understanding the causes of left-sided neck pain is crucial for proper diagnosis and treatment. Left-sided neck pain can result from several factors, including musculoskeletal issues, nerve compression, trauma, inflammation, or underlying medical conditions. Muscular strains, poor posture, and stress are common causes of neck pain. Additionally, conditions such as cervical disc herniation, cervical spinal stenosis, and osteoarthritis can lead to left-sided neck pain. According to global estimates, neck pain affects a significant portion of the population. In the United States alone, it has been reported that about 10% to 15% of individuals experience neck pain at any given time. Neck pain can occur in people of all ages, although it tends to be more prevalent in adults.
Read More About Pain In The Left Side Of The NeckStiff Neck
A painful stiff neck affects one in three people every year, and is most prevalent in the 35-49-year age group. It causes significant disability for all those affected, but is more commonly seen in women. A stiff neck can be a symptom of vascular disease, inflammatory disorders, infection, and malignancy. Therefore, it needs to be evaluated properly before any treatment begins. In this article, we’ll discuss what causes a painful stiff neck, how to diagnose it, and some common treatments.
Read More About Stiff NeckTingling Sensation in the Hands
Have you ever felt the sensation of a thousand tiny pins and needles pricking your hands or the subtle, electric tingling that runs down your fingers like a gentle current? Tingling sensations in the hands are more common than you might think and can be triggered by a multitude of factors, from temporary nerve compression to chronic medical conditions. While often dismissed as a momentary inconvenience, this seemingly innocuous tingling can sometimes be a signal from your body, a signpost pointing to underlying health concerns. In this article, we delve into the intriguing world of tingling sensations in the hands, unraveling the causes, potential implications, and, most importantly, what you can do to address them.
Read More About Tingling Sensation in the HandsCommon Causes Of Cervical Herniated Disc
Cervical disc herniations can have various causes, and some common factors that contribute to their development include:
- Genetics: Genetic factors can play a role in predisposing individuals to cervical disc herniations. Some people may have inherited traits that make their discs more susceptible to degeneration and herniation.
- Age-related wear and tear: As we age, the intervertebral discs in the cervical spine naturally undergo degenerative changes. The discs lose water content and elasticity, becoming less resilient and more prone to herniation.
- Poor posture: Prolonged periods of poor posture, such as slouching or forward head posture, can put excessive stress on the cervical discs. Over time, this can contribute to disc degeneration and increase the risk of herniation.
- Sedentary lifestyle: Lack of regular exercise and a sedentary lifestyle can weaken the muscles and supportive structures in the neck and back. Weak muscles provide less support to the spine, making it more susceptible to disc herniation.
- Heavy lifting: Lifting heavy objects improperly or using improper lifting techniques can strain the spine and increase the risk of disc herniation. The excessive load and improper mechanics can place excessive stress on the discs.
- Smoking: Smoking is associated with accelerated disc degeneration. It reduces the blood supply to the intervertebral discs, depriving them of essential nutrients and oxygen, which can contribute to disc degeneration and herniation.
- Obesity: Excessive body weight places increased stress on the cervical spine. The added weight can lead to increased pressure on the intervertebral discs, accelerating their degeneration and increasing the risk of herniation.
- Neck injury or trauma: Traumatic events, such as car accidents or sports injuries, can cause sudden and severe forces on the cervical spine, leading to disc herniation. Trauma can also cause structural damage to the discs, making them more susceptible to herniation.
- Degenerative disc disease: Degenerative disc disease refers to the natural wear and tear of the intervertebral discs over time. It involves the gradual breakdown of the discs, leading to disc degeneration, loss of disc height, and increased risk of herniation.
It is important to note that while these factors can increase the likelihood of cervical disc herniation, not everyone with these risk factors will develop herniations. A combination of these factors, along with other individual characteristics, lifestyle choices, and overall spinal health, contributes to the development of cervical disc herniations.
Diagnosing Cervical Herniated Discs
Imaging studies play a crucial role in diagnosing cervical disc herniations and providing valuable information about the location, extent, and impact of the herniation on the spinal structures. The utility of different imaging studies for diagnosing cervical disc herniations is as follows:
- X-rays: X-rays are often the initial imaging modality used for evaluating cervical spine conditions. While they do not provide detailed visualization of the soft tissues like discs,
X-rays can help identify other potential causes of symptoms, such as bone spurs, fractures, or spinal misalignment. X-rays are particularly useful in ruling out more serious conditions and assessing the overall alignment and stability of the cervical spine.
- Magnetic Resonance Imaging (MRI): MRI is considered the gold standard for evaluating cervical disc herniations. It provides detailed images of the soft tissues, including the intervertebral discs, spinal cord, nerves, and surrounding structures.
MRI can visualize the herniated disc, assess the degree of compression on neural structures, and help determine the appropriate treatment approach. It also helps identify other potential causes of symptoms and evaluate the overall health of the cervical spine.
- Computed Tomography (CT) scan: CT scans use X-rays and computer processing to create cross-sectional images of the cervical spine.
While CT scans provide less detailed visualization of soft tissues compared to MRI, they are valuable in evaluating the bony structures and detecting any fractures, bony abnormalities, or calcifications associated with the cervical disc herniation. CT scans are especially useful when there is a suspected bone-related issue or when MRI is contraindicated (e.g., patients with pacemakers or metal implants).
The choice of imaging study depends on several factors, including the patient’s symptoms, clinical presentation, and the suspected severity of the condition.
X-rays are often the initial screening tool, while MRI is typically used for confirming the diagnosis and assessing soft tissue involvement. CT scans are reserved for specific situations where bone-related abnormalities need to be evaluated in more detail.
It’s important to note that imaging studies should be interpreted in conjunction with the patient’s clinical history, physical examination findings, and symptoms to make an accurate diagnosis and determine the appropriate treatment plan. A healthcare professional, such as a radiologist or spine specialist, should interpret the imaging results and correlate them with the patient’s clinical presentation.
Common Treatments for Cervical Herniated Disc
With any injury, treatments are minimally invasive and progress to more invasive procedures over-time until you find success or improvement of your symptoms.
ACDF Surgery
ACDF stands for “anterior cervical discectomy and fusion.” It is a surgical procedure performed on the neck to relieve pressure on the spinal cord or nerve roots caused by a damaged or degenerated disc. During the procedure, the surgeon removes the damaged disc and replaces it with a bone graft or synthetic implant. Metal plates and screws may be used to hold the vertebrae together during the fusion process. ACDF surgery can help relieve symptoms such as neck pain, numbness, tingling, and weakness in the arms or hands caused by nerve compression in the neck. It is a commonly performed procedure…
Read More About ACDF SurgeryAnterior Cervical Discectomy And Fusion (ACDF) For Neck Pain
Anterior cervical discectomy and fusion (ACDF) surgery is a surgical procedure used to treat cervical radiculopathy in the neck region. It is also an effective treatment for those with severe neck pain due to spondylosis, tumors, fractures, and herniated discs. There are two stages of the ACDF surgery: discectomy and spinal fusion. In an anterior cervical discectomy and fusion surgery, the diseased disc is first removed and a bone graft is inserted in its place. The graft is then held in place by a plate and fused with the cervical vertebra above and below.
Read More About Anterior Cervical Discectomy And Fusion (ACDF) For Neck PainArtificial Cervical Disc Replacement Surgery
Also known as cervical disc replacement is a surgical procedure designed to alleviate neck pain and other symptoms caused by a herniated disc, annular tears, and degenerative discs that fail conservative treatments. While this technology is still new, the promise from surgeons and the companies that are producing the device touted it as a solution to the ASD – adjacent segment disease that comes with fusion of the cervical spine. In reality, that didn’t happen, but it has reduced ASD. Research has shown that ACDF (anterior cervical discectomy with fusion) can result in ASD 7-8 out of 10 times.
Read More About Artificial Cervical Disc Replacement SurgeryCervical Disc Replacement
Cervical disc arthroplasty (CDA), also known as cervical disc replacement, is a surgical procedure used to treat cervical disc disease. The procedure involves removing the damaged or degenerated intervertebral disc in the cervical spine and replacing it with an artificial disc device. CDA is typically performed for patients with symptomatic cervical disc disease, such as disc herniation, degenerative disc disease, or spinal stenosis. The procedure is intended to relieve symptoms such as neck pain, arm pain, and numbness or tingling in the arms or hands. CDA is considered a less invasive and more motion-preserving alternative to traditional cervical spinal fusion surgery…
Read More About Cervical Disc ReplacementCervical Epidural Steroid Injection
The neck pain started out as a dull ache but steadily progressed. It becomes constant and oftentimes keeps you up at night. Turning your head can send an electrical current down your arm. Rest, medications and physical therapy failed to provide much relief. Your doctor referred you to a pain clinic for a Cervical Epidural steroid injection. The injection was performed at an ambulatory surgical center. Unfortunately, the pain is now worse. What is a Cervical Epidural injection? Are there different types of Cervical Epidural injections? What are…
Read More About Cervical Epidural Steroid InjectionPRP Injections
PRP is short for platelet-rich plasma, and it is autologous blood with concentrations of platelets above baseline values. The potential benefit of platelet-rich plasma has received considerable interest due to the appeal of a simple, safe, and minimally invasive method of applying growth factors. PRP treatments are a form of regenerative medicine that utilizes the blood healing factors to help the body repair itself by means of injecting PRP into the damaged tissue. In regenerative orthopedics, it is typically used for the treatment of muscle strains, tears, ligament and tendon tears, minor arthritis, and joint instability. There have been more than 30 randomized controlled trials of PRP…
Read More About PRP InjectionsRegenexx® Alternatives to Back & Neck Surgery
Regenexx has a range of procedures developed to help patients avoid spine surgery and the side effects of epidural steroid injections.
These procedures utilize the patient’s own natural growth factors or bone marrow concentrate containing stem cells to treat bulging or herniated discs, degenerative conditions in the spine, and other back and neck conditions that cause pain. Click this page to learn more.
Complications and Risks of Cervical Disc Surgery
Cervical disc surgery, like any surgical procedure, carries potential risks and complications. Although complications are relatively rare, it’s important to be aware of the possible risks.
Some potential complications of cervical disc surgery include:
- Infection: There is a risk of infection at the surgical site or in the surrounding tissues. This can usually be treated with antibiotics, but in some cases, additional surgical intervention may be required.
- Bleeding: Excessive bleeding can occur during or after surgery. In rare cases, it may require a blood transfusion or further surgical intervention to control the bleeding.
- Nerve or spinal cord injury: During the surgery, there is a small risk of damage to nearby nerves or the spinal cord, which can result in temporary or permanent neurological defects. The risk of such injuries is generally low.
- Persistent or increased pain: Some patients may experience persistent or increased pain following cervical disc surgery. This could be due to various factors, such as nerve irritation, scar tissue formation, or incomplete resolution of the underlying problem.
- Hoarseness or difficulty swallowing: The surgical approach used for cervical disc surgery may involve moving or retracting the esophagus or laryngeal nerves, which can lead to temporary hoarseness or difficulty swallowing. These symptoms usually resolve on their own.
- Instrumentation-related complications: If cervical fusion is performed, complications associated with the hardware used (such as plates, screws, or cages) can occur. These include hardware loosening, fracture, or migration.
- Blood clots: There is a small risk of developing blood clots (deep vein thrombosis) in the legs, which can potentially travel to the lungs (pulmonary embolism). Measures such as early mobilization and blood thinners may be used to prevent this.
It’s essential to discuss these potential complications and their likelihood with your surgeon before undergoing cervical disc surgery. Surgeons will take appropriate precautions to minimize the risks and maximize the chances of a successful outcome.
Is Surgery Necessary?
Surgery is only suggested when there is neurologic compromise such as progressive weakness or bowel / bladder incontinence. Pain, no matter how severe, does not necessitate surgery before all alternative treatments have been attempted.
Once you have surgery, the spine is never the same. At the same time, if the surgery fails to treat pain, it can lead to chronic pain and other complications.
Rehabilitation and Physical Therapy for Cervical Herniated Discs
Therapy is important for individuals with disc herniations as it helps manage pain, avoid surgery, and rehabilitate after surgery if necessary. It provides education, promotes self-management, and improves mobility, functionality, and strength.
Therapy also addresses psychological well-being and empowers individuals to actively participate in their recovery and prevent future injuries.
Coping Strategies And Lifestyle Changes
Coping strategies and lifestyle changes can be helpful in managing disc herniations.
Here are some key approaches:
- Pain management techniques: Utilize techniques such as heat or cold therapy, gentle stretching, relaxation exercises, and over-the-counter pain medications to help alleviate pain and discomfort.
- Correct body mechanics: Practice proper body mechanics during activities such as lifting, bending, and sitting. This involves using the legs instead of the back, maintaining good posture, and avoiding repetitive or prolonged activities that may strain the spine.
- Weight management: Maintain a healthy weight or work towards achieving a healthy weight to reduce the strain on the spine and minimize pressure on the discs.
- Exercise and physical activity: Engage in regular low-impact exercises, such as walking, swimming, or cycling, to improve strength, flexibility, and overall fitness. Focus on exercises that strengthen the core muscles and support the spine.
- Posture and ergonomics: Pay attention to maintaining good posture while sitting, standing, and performing daily activities. Use ergonomic principles, such as ergonomic chairs and proper desk setup, to reduce strain on the spine during prolonged sitting or computer work.
- Avoid smoking: Smoking can impair the healing process and decrease blood flow to the spine, potentially exacerbating disc herniation symptoms. Quitting smoking or avoiding exposure to tobacco smoke can contribute to better healing and overall spine health.
- Stress management: Develop effective stress management techniques, such as relaxation exercises, deep breathing, meditation, or engaging in hobbies and activities that promote relaxation and mental well-being. High stress levels can contribute to muscle tension and exacerbate pain.
- Adequate rest and sleep: Ensure you are getting sufficient rest and practicing good sleep hygiene. Sleep is essential for the body’s healing and recovery processes.
- Proper nutrition: Maintain a balanced diet rich in nutrients to support overall health and provide essential building blocks for tissue healing and repair.
- Regular check-ups: Stay in touch with healthcare professionals to monitor your condition, receive guidance on managing symptoms, and address any concerns that may arise.
Remember, it’s important to consult with healthcare professionals, such as orthopedic specialists or physical therapists, who can provide personalized recommendations and guidance tailored to your specific needs and condition.
Don’t Let Cervical Herniated Discs Hold Your Life Back
Cervical disc herniations do not have to be the end of the road. There exists a multitude of options. If you have been dealing with a disc herniation and are contemplating surgery, call and set up an evaluation with one of our experts who can further evaluate you and your candidacy for a surgery avoidance.

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics.
Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who travel to Colorado to undergo innovative, non-surgical treatments. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine. Dr. Centeno has also served as editor-in-chief of a medical research journal dedicated to traumatic injury.
Dr. Centeno trained at the Baylor College of Medicine, Texas Medical Center, and the Institute for Rehabilitation Research. He hails from both Florida and New York and currently resides in Boulder, Colorado with his wife and three children.

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…
Read more
John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.
Read more
Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.
Read more
Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Read moreAre you a candidate?
Other Resources for Herniated Cervical Disc
-
Learn Why Your Neck Hurts
Globally, neck pain is estimated to affect 203 million people, making it one of the most common musculoskeletal pains worldwide. It often stems from a combination of factors, such as muscle strain, poor posture, and degenerative disc conditions. This pain can limit movement, disrupt daily life, and, in severe cases, impact overall health. While some…
-
What Happens If You Have Back Pain From Golf?
Back pain is a common complaint among golfers, impacting both amateur enthusiasts and professional athletes. Golf, while seemingly low-impact, involves repetitive, high-intensity movements that can stress the spine and surrounding structures. Understanding the causes, symptoms, and preventative measures for golf-related back pain can help maintain performance and long-term health. Golf And Back Pain The golf…
-
The C1 And C2 Vertebrae – What To Know
The C1 and C2 vertebrae, also known as the atlas and axis, are the uppermost bones in the spinal column. They play a crucial role in supporting the skull and enabling head movements. Damage or injury to these vertebrae often leads to pain, limitations to daily activities, and reduced quality of life. Many patients, without…
-
All You Need to Know about the L4 Vertebra
The L4 vertebra is one of the five vertebrae in the lower back, located just above the sacrum. It plays a crucial role in supporting the upper body’s weight and enabling movement. Injury or degenerative changes that affect the L4 vertebra can lead to chronic pain and mobility issues. Many patients often rely on medications…
-
Spinal Fusion Recovery: What to Expect
Navigating spinal fusion recovery can be a daunting prospect, given its impact on daily life and mobility. Understanding what to expect during this process is crucial for individuals undergoing this procedure. In this article, we’ll explore the typical timeline, challenges, and strategies for managing recovery after spinal fusion surgery, providing insights to help individuals prepare…
-
Back Cracking: The Truth of What’s Actually Happening in Your Body
Back cracking is a phenomenon that many people experience, often eliciting both curiosity and concern. Whether it’s the satisfying pop from a morning stretch or the deliberate twist during a yoga session, the sound and sensation of cracking your back can be oddly gratifying. But what exactly is happening inside your body when you hear…