Knee Clicking
Get Help With Knee ClickingYou hear it as you walk down the stairs. The clicking in your knee is increasing! Your PCP simply dismisses it as part of aging but you are concerned. What are the major causes of clicking in the knee? When should I be concerned about it? How do I get my knee to stop clicking? Let’s dig in.
5 Major Causes of Clicking in Knee
Clicking in the knee can occur for a number of reasons. The 5 major causes include:
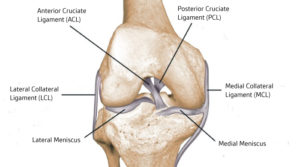
Ligament Injuries
A ligament is a thick piece of connective tissue that connects one bone to another. The knee has 4 principal ligaments: ACL, PCL, MCL, and LCL. Ligaments provide important stability for the knee (1). If injured or torn, ligaments can create instability. This instability can cause clicking in the knee. As ligaments travel across boney surfaces they can also catch make the knee click.
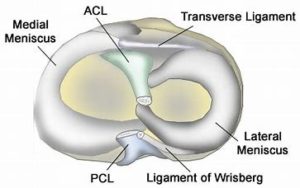
Meniscus Tear
The meniscus is a C-shaped cushion situated between the thigh bone and shin bone. Each of us has two menisci per knee. One on the inside (medial) and one on the outside (lateral) of the knee. The meniscus functions as a shock absorber and joint stabilizer and is susceptible to injury. Meniscus tears are among the most common knee injuries. There are many different types of meniscus tears that are classified (2). Examples include horizontal, vertical, and complex Risk factors for meniscus tears include advanced age, male gender, work-related kneeling, and climbing stairs (3). Injury to the meniscus can cause clicking in the knee that is often times associated with pain.
Osteoarthritis
Osteoarthritis is the most common form of arthritis. It is a joint disease where the cartilage that lines and protects the joint gradually wears down resulting in pain, swelling, and restriction in movement. Approximately 13% of women and 10% of men aged 60 years and older have symptomatic knee osteoarthritis (4). Risk factors for knee osteoarthritis include obesity, female gender, repetitive knee trauma, muscle weakness, squatting, and meniscus injuries (5). Loss of cartilage and knee swelling can cause clicking in the knee.
Patellofemoral Syndrome
Patellofemoral syndrome, also known as runner’s knee is a medical condition where there is a misalignment of the kneecap. The kneecap is intended to smoothly glide up and down a boney groove in the thigh bone. The thigh bone is also known as the femur. The knee cap is sometimes called the patella. In patellofemoral syndrome, the knee cap no longer tracks smoothly in the boney groove. As a result of misalignment, the knee cap rubs repetitively against the boney wall with injury to the cartilage, ligaments, and tendons. These injuries oftentimes result in knee clicking and/or pain and swelling.
Soft Tissue/Scar Tissue
Surgery or significant trauma can cause soft tissue in the knee to become injured and inflamed. In addition, scar tissue can also develop. Both soft tissue injury and scar tissue can cause knee clicking. It is extremely common during the first year after knee surgery due to these two factors.
When Should I be Concerned About Clicking in Knee?
Infrequent clicking in the knee that is not associated with other symptoms typically does not warrant concern or further evaluation. Clicking in the knee that is increasing in frequency and associated with any of the following symptoms warrants further evaluation.
- Pain
- Swelling
- Locking episodes
- Limited range of motion
Who should evaluate the clicking in your knee? Bypass your surgeon and schedule a consultation with a physician trained in interventional orthopedics. Surgeons provide surgical solutions that are not always in your best interest. What is interventional orthopedics? It is a board-certified physician in PM& R or anesthesia with advanced orthopedic training with nonsurgical treatment options. They use orthobiologics to heal injured orthopedic tissue. Orthobioligcs are biological substances naturally found in the body that are used to promote quicker healing of muscle, tendon, and bone injuries. To learn more please click on the video below.
How Do I Get my Knee to Stop Clicking?
Identifying the underlying cause of the clicking in the knee will provide the best clinical results. Conservative therapy when appropriate is always the first line of treatment.
ACL Tears
The Anterior Cruciate Ligament (ACL) is one of four major ligaments in the knee. It is an important stabilizer of the knee and prevents the shin bone (tibia) from sliding in front of the thigh bone (femur). The ACL is susceptible to injury. It is most likely to be injured during activity or by impact. A torn ACL is a common injury for athletes at all levels, but it is most common for people who are active or who experience impact injuries to the knee. ACL injuries can happen to anyone of any age, condition, or ability, and it can be injured in many ways. Examples include abruptly changing direction, slowing down while running, landing incorrectly, or getting struck by someone or some object.
Read More About ACL TearsBaker’s Cyst
A Baker’s cyst can cause knee pain. A Baker cyst is swelling caused by fluid from the knee joint protruding to the back of the knee. They are NOT a true cyst since it has communication with the synovial sac. They typically arise from degenerative changes or injury to the articular cartilage (arthritis) or meniscus. At the Centeno-Schultz Clinic, we believe that baker’s Cysts are simply a barometer of the health of the knee joint. In a healthy knee, there are absent whereas with injury and degenerative changes they are common. They arise between the tendons of the medial head…
Read More About Baker’s CystBone Spurs In The Knee
Bone spurs, also known as osteophytes, are abnormal growths that can form along any bony surface in the body. They most frequently occur where tendons and ligaments attach to the bone. As a result, they are more commonly seen in large mobile joints that support weight, such as the hips, spine, ankles, or knees. Surprisingly, most bone spurs are relatively benign but are a clinical sign of instability in the area. Research demonstrates that if a ligament has laxity, the constant strain at the insertion into the bone will elevate the surface of the bone, creating additional bone formation – this is known as a traction osteophyte.
Read More About Bone Spurs In The KneeChondromalacia
Chondromalacia is the knee usually causes pain, typically around the kneecap or deep in the kneecap. You can also have some grinding sensations or crepitus which are sounds and noises coming from around the knee with certain motions. Typically, pain and grinding sensations are worse with bending the knee, especially for prolonged periods of time, kneeling on the knee, walking downstairs, or running downhill. Standing after prolonged sitting or an immobility period where the knee is bent can cause some discomfort as well. Some people may experience swelling, others may experience locking or catching in the knee, feeling the knee wants to give out, or a feeling of weakness….
Read More About ChondromalaciaHamstrings Tendinopathy
Hamstring tendinopathy, a condition that causes pain and tenderness in the hamstring tendons, represents a common but often misunderstood musculoskeletal issue. It typically occurs in athletes and individuals engaged in high-intensity activities but isn’t limited to them. This condition, including its more specific form, high hamstring tendinopathy, can significantly impact daily and athletic performance, making understanding its nuances critical.
Read More About Hamstrings TendinopathyIliotibial Band Syndrome (ITBS)
Also known as “IT Band Syndrome” also known as “ITB Syndrome,” iliotibial band syndrome is a painful medical condition that affects the lateral hip, leg, and knee. It can affect individuals of all ages and most often is caused by repetitive activities like running, cycling, hiking, and walking. Your iliotibial band is a thick band of connective tissue that runs from the outside of your hip down to the outside aspect of your knee. Its principal function is to stabilize the hip and knee. If it becomes tight and dysfunctional, you may experience pain along with this band of tissue due to strain or inflammation. You may also experience pain, limited range of motion in…
Read More About Iliotibial Band Syndrome (ITBS)Knee Arthritis
In the human body, a joint is simply where 2 ends of bone come together. At the ends of these bones, there is a thick substance called “Hyaline Cartilage” that lines the ends. Hyaline cartilage is extremely slippery which allows the two ends of the bone to slide on top of each other. Then there is a capsule that connects the two ends filled with “synovial fluid” that acts as a further lubricant to make it more slippery! Arthritis in the knee is defined by loss of the hyaline cartilage plus other changes that happen to the bone such as additional bone being laid down (bone spurs/osteophytes). The cartilage layer is worn down to the point of exposing the underlying bone they cover…
Read More About Knee ArthritisKnee Instability
Knee instability is a condition that results when the knee joint is unstable and does not move or function normally. This can cause the knee to feel like it is going to give out or buckle. Knee instability can be caused by a variety of factors, including trauma or injury to the knee, ligament injury, arthritis or other degenerative diseases of the knee, weakness or instability of the muscles around the knee, muscle atrophy, injury to another joint in the body creates an imbalance. Knee stability, and stability in general, is very important. Lack of knee stability can lead to more problems over time, such as pain and arthritis…
Read More About Knee InstabilityLCL Sprain
What is an LCL Sprain? A strain or tear to the lateral collateral ligament (LCL) is known as an LCL injury. The LCL is a band of tissue that runs along the outer side of your knee. It aids in keeping the bones together while you walk, ensuring that your knee joint remains stable. How you feel and what type of treatment you’ll require depends on how severely your LCL has been stretched or torn. If it’s only a minor sprain, self-care at home might help. However, if it’s a significant tear or sprain, you may need physical therapy, an injection-based procedure, or surgery….
Read More About LCL SprainLCL Tear
A strain or tear to the lateral collateral ligament (LCL) is known as an LCL injury. The LCL is a band of tissue that runs along the outer side of your knee. It aids in keeping the bones together while you walk, ensuring that your knee joint remains stable. How you feel and what type of treatment you’ll require depends on how severely your LCL has been stretched or torn. If it’s only a minor sprain, self-care at home might help. However, if it’s a significant tear, you may need physical therapy, an injection-based procedure, or surgery. Orthopedists categorize LCL tears into 3 grades…
Read More About LCL TearMCL Sprain
The medial collateral ligament AKA MCL is a thick, strong band of connective tissue on the inside portion of your knee. It connects the top part of the tibia (shin) to the bottom part of the femur (thigh). This is a vital ligament that works along the lateral collateral ligament (LCL), anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL) to bring stability, structure, and movement to the knee. The MCL provides support and stability for the inside (medial) aspect of the knee. MCL sprains are a common injury in sports such as football, hockey, and skiing. The ligament can…
Read More About MCL SprainMCL tear
The medial collateral ligament AKA MCL is a thick, strong band of connective tissue on the inside portion of your knee. It connects the top part of the tibia (shin) to the bottom part of the femur (thigh). This is a vital ligament that works along the lateral collateral ligament (LCL), anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL) to bring stability, structure, and movement to the knee. The MCL provides support and stability for the inside (medial) aspect of the knee. MCL tears are a common injury in sports such as football, hockey, and skiing. The ligament can…
Read More About MCL tearMeniscus Tears
The meniscus is a c-shaped piece of cartilage in the knee that functions as an important shock absorber. It is sandwiched between the thigh and shin bone. There are two menisci per knee. One on the inside portion of the knee (medial) one on the outside aspect (lateral). The knee meniscus is susceptible to injury. The most common injury is a tear in the meniscus. Not all meniscus tears however cause pain. When symptomatic a meniscus tear can cause pain, swelling, and restriction in range of motion. Tears in the knee meniscus can arise from trauma or degeneration. There are many different types of meniscus tears based upon locations….
Read More About Meniscus TearsPatellar Tendon Tear
The Patellar tendon is the thick connective tissue that starts at the base of the kneecap (Patella) and extends down to the shin. The is an extension of the Quadriceps tendon (1). The Quadricep is the large thick muscle that is often referred to as our thigh. The Patellar tendon works together with the Quadriceps muscle to straighten (extend) the knee. It is easy to touch your Patellar tendon as it is immediately below the knee cap. There are many different causes of Patellar tendon tears. Patellar tendon tears are a common sport injury but can also occur from overuse or a motor vehicle injury…
Read More About Patellar Tendon TearPatellar Tendonitis
What is the Patellar Tendon? A tendon is a piece of connective tissue that connects muscle to bone. It serves to move the bone or a given joint. The patellar tendon is a major tendon in the knee. It is located at the bottom of the kneecap (patella) and stretches down to the shin. The patellar tendon enables you to extend your knee, kick, run, and jump. What is Patellar Tendinitis? Patellar tendinitis is an irritation and inflammation of the tendon that connects your kneecap (patella) to your shinbone. Patellar tendinitis, also known as jumper’s knee, can affect anyone. The most common symptom is pain at the shin or lowest part of the kneecap…
Read More About Patellar TendonitisPatellofemoral Pain Syndrome
Patellofemoral pain syndrome (PFS), also called runner’s knee or retropatellar pain syndrome, is a significant cause of pain in the front of the knee. The pain is usually experienced behind or around the patella (kneecap) when the knee is bent or fully loaded. This post discusses everything you need to know about patellofemoral pain syndrome.
Read More About Patellofemoral Pain SyndromePCL Sprain
The Posterior Cruciate Ligament is one of the paired ligaments in the middle of the knee. It is made up of 2 separate bundles: The two bundles of the PCL, and the ALB (anterior lateral bundle), and the PMB (posterior medial bundle), function synergistically to provide stability. The PCL functions as one of the main stabilizers of the knee joint and serves primarily to resist excessive posterior translation of the tibia relative to the femur. The PCL also acts as a secondary stabilizer of the knee preventing excessive rotation specifically between 90° and 120° of knee flexion. A PCL sprain happens when force is applied beyond…
Read More About PCL SprainPCL Tear
The Posterior Cruciate Ligament (PCL) is a paired ligament in the middle of the knee. It is made up of two separate bundles: ALB (anterior lateral bundle) and PMB (posterior medial bundle). These bundles work synergistically to provide stability. The PCL plays an important stabilizing role in the knee joint by resisting excessive posterior translation of the tibia relative to the femur. Between 90 and 120 degrees of knee flexion, it serves as secondary support for preventing excessive rotation. PCL tears happen when force is applied beyond what the PCL tensile strength is capable of resisting. The tensile strength of the PCL is well documented…
Read More About PCL TearPes Anserine Bursitis
Knee pain located at the lower inside of the knee can be caused by Pes Anserine Bursitis, which is irritation of the tendons that run on the inside aspect of the knee. Commonly mistaken for arthritic pain, meniscal pain, and sometimes nerve pain from the low back! Don’t be misdiagnosed, and let’s dive in below to get a better understanding of Pes Anserine Bursitis. The Pes Anserine Bursa is a bursa that surrounds 3 tendons of the leg. A bursa is a thin, slippery, sac-like film that contains a small amount of fluid. A bursa is found between bones and soft tissues in and around joints…
Read More About Pes Anserine BursitisRadial Meniscus Tears
The meniscus is an important fibro-cartilage structure within the knee that absorbs shock and provides cushioning. It has a semicircular ‘C’ shape and sits between the femur (thigh bone) and the tibia (lower leg bone). The meniscus protects the two bony structures from weight, shock, and shear forces. Each knee contains two menisci, one on the outside (lateral) and one inside (medial).
Read More About Radial Meniscus TearsLigament Injuries
Ligament injuries, also known as sprains are common in patients with active lifestyles. There are three grades of sprains.
- Grade 1: ligament is stretched but intact
- Grade 2: partial tear of the ligament
- Grade 3: complete tear
Grade 3 injuries require surgery. Steroids are to be avoided as they are toxic to ligaments and can potentially cause additional damage (6). Treatment options include PRP and a patient’s own bone marrow-derived stem cells. The Centeno-Schultz Clinic’s doctors are experts in the treatment of ligament injuries. We pioneered the use of bone marrow stem cells in the nonsurgical treatment of ACL tears allowing patients to forgo the risks and complications of traditional ACL graft surgery. The risks of the ACL graft surgery are significant and include a 6x risk of re-tear within 24 months post-surgery (7) and development of arthritis (8).
Meniscus tear
Not all meniscus tears are painful. In fact, in one study 60% of patients without pain had meniscus tears on MRI. PRP is effective in the treatment of meniscus tears. Steroids should be avoided as they are toxic. Meniscus surgery has been demonstrated to be no better than PT (9). In addition, it increases the risk of knee instability and arthritis. To learn more about the treatment of meniscus tears please click on the video below.
Osteoarthritis
Knee osteoarthritis is common but does not need to keep you on the sidelines. Mild arthritis can be treated with PRP whereas more advanced cases require bone marrow stem cells. Knee replacement is major surgery with significant risks and complications. Risks include the need for a second surgery in 6% of patients (10) and patients who undergo knee are 9 times more likely to have a heart attack (11).
Patellofemoral Syndrome
Treatment of patellofemoral syndrome starts with physical therapy. The focus is on improving the tracking of the patella through select muscle strengthening. Loose or damaged knee ligaments can be treated with ultrasound-guided injections of PRP. Oftentimes patients with patellofemoral syndrome also have a lumbar disc and nerve injury that aggravates their knee condition.
In Conclusion
Clicking in the knee can be frustrating. The 5 major causes of this are ligament injuries, meniscus tears, knee osteoarthritis, patellofemoral syndrome, and soft tissue. If infrequent and not associated with other symptoms typically does not warrant further evaluation. If it is increasing in frequency and associated with pain, swelling, locking episodes, and limited range of motion evaluation is indicated. The clicking is a warning sign that you have a problem that needs attention. Surgeons provide surgical solutions. A physician trained in Interventional Orthopedics can provide you with a range of nonsurgical treatment options. Treatment for this requires the underlying cause to be identified. The Centeno-Schultz Clinic Physicians are experts in the treatment. Treatment options include PRP and stem cell injections.
If the clicking in the knee is increasing and associated with pain, swelling, or limited range of motion this is a warning sign. Act now before the problem gets bigger and the options are limited. Schedule a Telemedicine consult with a board-certified physician who can review your history, studies, and provide you with the best nonsurgical treatment option. Listen to your body as it is warning you!
References
1.Hastings DE. Diagnosis and management of acute knee ligament injuries. Can Fam Physician. 1990;36:1169-1189.
2. Mordecai SC, Al-Hadithy N, Ware HE, Gupte CM. Treatment of meniscal tears: An evidence-based approach. World J Orthop. 2014;5(3):233-241. Published 2014 Jul 18. doi:10.5312/wjo.v5.i3.233.
3. Snoeker BAM, Bakker EWP, Kegel CAT, Lucas C. Risk factors for meniscal tears: a systematic review including meta-analysis. J Orthop Sports Phys Ther 2013;43:352-367.
4. Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian J Intern Med. 2011;2(2):205-212.
5. Yoshimura N, Muraki S, Oka H, Kawaguchi H, Nakamura K, Akune T. Association of knee osteoarthritis with the accumulation of metabolic risk factors such as overweight, hypertension, dyslipidemia, and impaired glucose tolerance in Japanese men and women: the ROAD study. J Rheumatol. 2011;38(5):921-930. doi:10.3899/jrheum.100569.
6. Wernecke C, Braun HJ, Dragoo JL. The Effect of Intra-articular Corticosteroids on Articular Cartilage: A Systematic Review. Orthop J Sports Med. 2015;3(5):2325967115581163. Published 2015 Apr 27. doi:10.1177/2325967115581163
7. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of Second ACL Injuries 2 Years After Primary ACL Reconstruction and Return to Sport. Am J Sports Med. 2014;42(7):1567-73.doi: 10.1177/0363546514530088.
8.Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049-57. DOI: 10.1177/0363546514526139.
9.Collins JE, Losina E, Marx RG, et al. Early Magnetic Resonance Imaging-Based Changes in Patients With Meniscal Tear and Osteoarthritis: Eighteen-Month Data From a Randomized Controlled Trial of Arthroscopic Partial Meniscectomy Versus Physical Therapy. Arthritis Care Res (Hoboken). 2020;72(5):630-640. doi:10.1002/acr.23891
10. Pabinger C, Berghold A, Boehler N, Labek G. Revision rates after knee replacement. Cumulative results from worldwide clinical studies versus joint registers. Osteoarthritis Cartilage. 2013 Feb;21(2):263-8. doi: 10.1016/j.joca.2012.11.014.
11. Lu N, Misra D, Neogi T, Choi HK, Zhang Y. Total joint arthroplasty and the risk of myocardial infarction: a general population, propensity score-matched cohort study. Arthritis Rheumatol. 2015;67(10):2771–2779. doi: 10.1002/art.39246