Thoracic Radiculopathy
CAUSES, SYMPTOMS, TREATMENT OPTIONS, AND OTHER RESOURCES
Thoracic radiculopathy is a painful medical condition that affects both men and women alike. Pain, paresthesia, decreased sensation, and weakness are the major symptoms. Radiculopathy refers to the whole complex of symptoms that can be caused by irritation or compression of a nerve root in the spine. Thoracic radiculopathy is irritation or compression of a thoracic spinal nerve. Common causes of radiculopathy in the thoracic region are thoracic disc injuries, thoracic facet arthritis, ligament thickening, facet cyst, unstable rib attachments, and bone spurs. Diagnosis of thoracic radiculopathy can be difficult. Treatment options vary depending upon the severity and when appropriate should always start with conservative care.
An Overview With Dr. John Schultz
Where In The Thoracic Spine Does It Hurt?
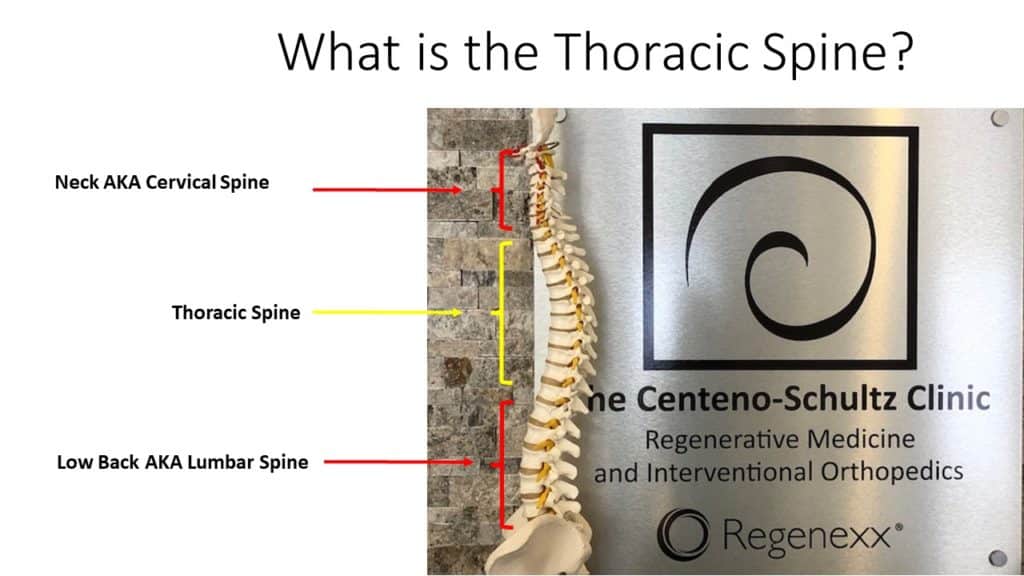
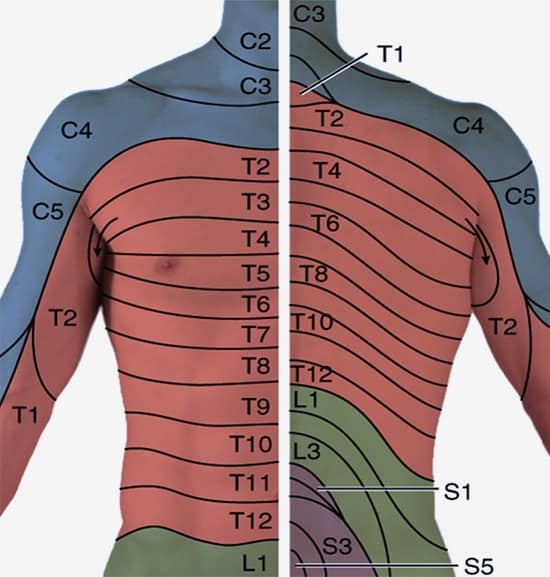
The thoracic spine is that part of the spine that is below the neck and above the low back. Oftentimes it is referred to as mid-back. It consists of 12 boney building blocks that stack one upon another (vertebral bodies). Sandwiched between the boney building blocks is an important shock absorber called a disc. There are 12 pairs of ribs in the body: right and left. At each level of the spine, a rib joins the spine forming a joint termed the costotransverse joint (CTJ). Thoracic nerves exit the spinal canal at each level of the spine. Each thoracic nerve corresponds with a specific area in the spine as illustrated below.
Irritation or compression of a thoracic spinal nerve can cause pain and altered sensation along the nerve’s path. The pain can be local or radiate:
- Up into the neck
- Across the chest wall
- Down into the low back
Painful Symptoms Of Thoracic Radiculopathy
Pain is common with thoracic radiculopathy and can vary in location and intensity depending on the location and severity of the actual nerve irritation or injury. Pain can be mild, moderate, or severe. Onset may be gradual or abrupt in nature. The pain can be localized or present as:
- Scorching or shooting pain in the ribs, side, or abdomen
- Band-like pain
- Pain in the chest and torso
Other symptoms
Back Pain in Ribs
Experiencing thoracic spine and rib pain? Learn more about what could be causing this and the treatment options that can provide lasting relief. Back pain in the ribs can be a common and often debilitating condition, causing discomfort and limiting mobility for many individuals. The pain can range from mild to severe and may be caused by various underlying conditions. Understanding the many causes of rib and back pain is important and can assist in securing an accurate diagnosis. Treatment options vary depending on the underlying cause and severity of symptoms.
Read More About Back Pain in RibsBig Toe Numbness
Believe it or not, one of those significant issues that can present as numbness stems from the low back. In the lumbar spine, the nerve that exits the spine at the L5 level branches down through the hip, thigh, knee, lower leg, and, yes, all the way into the foot and toes. So a pinched or irritated nerve at that L5 level in the back can create problems, such as pain, numbness, tingling, and so on, anywhere along the nerve branch. So what can irritate the L5 spinal nerve? The list is long, but it includes disc issues, such as herniated…
Read More About Big Toe NumbnessLeft Arm Numbness
Treatment depends upon the underlying cause of the arm numbness. Left-arm numbness is a warning sign that requires attention. As noted above unexplained numbness requires immediate attention. At the Centeno-Schultz Clinic, we are experts in the treatment of left-arm numbness due to cervical nerve irritation, cervical stenosis, thoracic outlet syndrome, and peripheral nerve injuries. When appropriate first-line treatment should involve conservative care including physical therapy and stretching. Steroid injections should be avoided as they are toxic to orthopedic tissue and can accelerate damage. Surgery for Cervical Stenosis and Thoracic…
Read More About Left Arm NumbnessReferred Pain From The Thoracic Spine
Pain is the body’s way of signaling distress or injury. But what if your body manifests pain in a certain area of your body and yet the actual source of the discomfort is a completely different part of your body? In this article, we will explore the intricacies of referred pain, specifically referred pain from the thoracic spine. We’ll explore what this typically feels like, what conditions commonly cause referred pain, and the treatment options available to treat the root cause of this symptom.
Read More About Referred Pain From The Thoracic SpineThoracic Spine Pain
Simply put thoracic spine pain is pain that arises from the thoracic spine. It may be acute or chronic. It may be constant or intermittent. It may be mild or can be so severe as to take your breath away. To better understand thoracic spine pain please review the sections below. The thoracic spine is that part of the spine that is sandwiched between the neck and low back. Many refer to it as the middle section of your spine. It starts at the base of your neck and ends at the bottom of your ribs. The thoracic spine is the longest region in the spine.
Read More About Thoracic Spine PainThoracic Spine Tightness
Thoracic spine tightness can be caused by a number of different conditions. Many providers and medical practices focus on treating symptoms, with the aim of reducing them. Therefore, they provide prescriptions for different medications and referral to physical therapy with the hope that this will reduce or eliminate symptoms. At the Centeno-Schultz Clinic, we take a different approach. We believe that the first step is an accurate diagnosis. By identifying the accurate underlying issue, patients can receive the appropriate therapy and get the best clinical results. The process starts with a board-certified, fellowship-trained physician taking a detailed history that includes the onset of symptoms, presence or absence of trauma, aggravating factors, alleviating factors, and treatment to date.
Read More About Thoracic Spine TightnessUpper Back Pain Between The Shoulder Blades
Upper back pain between the shoulder blades is also known as interscapular pain. Fifteen percent of the population suffers from chronic upper back pain. Finding the source of interscapular pain can be tricky because the upper back houses many important structures like the heart, the upper lobes of the lung, the cervical spine, the scapulas, and a dozen or so of muscles and nerves.
Read More About Upper Back Pain Between The Shoulder BladesAbnormalities Caused By Thoracic Nerve Damage
Irritation or compression of a thoracic nerve can cause a number of different signs and symptoms. The symptoms and their intensity depend upon many factors including the location of the nerve injury, its severity, and whether it is acute or longstanding. Common abnormalities include:
Paresthesia
This is defined as an abnormal sensation, typically tingling, pricking (“pins and needles”), or even a burning sensation along the path of the nerve.
Hypoesthesia
Abnormally decreased sensitivity, particularly to touch, characterizes this symptom.
Anesthesia
It is defined as insensitivity to pain and is characterized by motor loss, pain, and stiffness.
Weakness
Irritation or compression of a nerve can lead to muscle weakness and atrophy.
Causes Of Radiculopathy In The Thoracic Region
At each level of the spine, a nerve exits the spinal cord through a boney doorway called the neuroforamen. Foramen means door. Hence a neuroforamen refers to the doorway through which the nerve exits the spinal cord along its path to different structures in the body. There are multiple structures surrounding the exiting thoracic nerve root which can narrow its path. If significant, the narrowing can cause irritation and or compression of the nerve. This narrowing when severe is referred to as foraminal stenosis. Common causes of radiculopathy in the thoracic spine include:
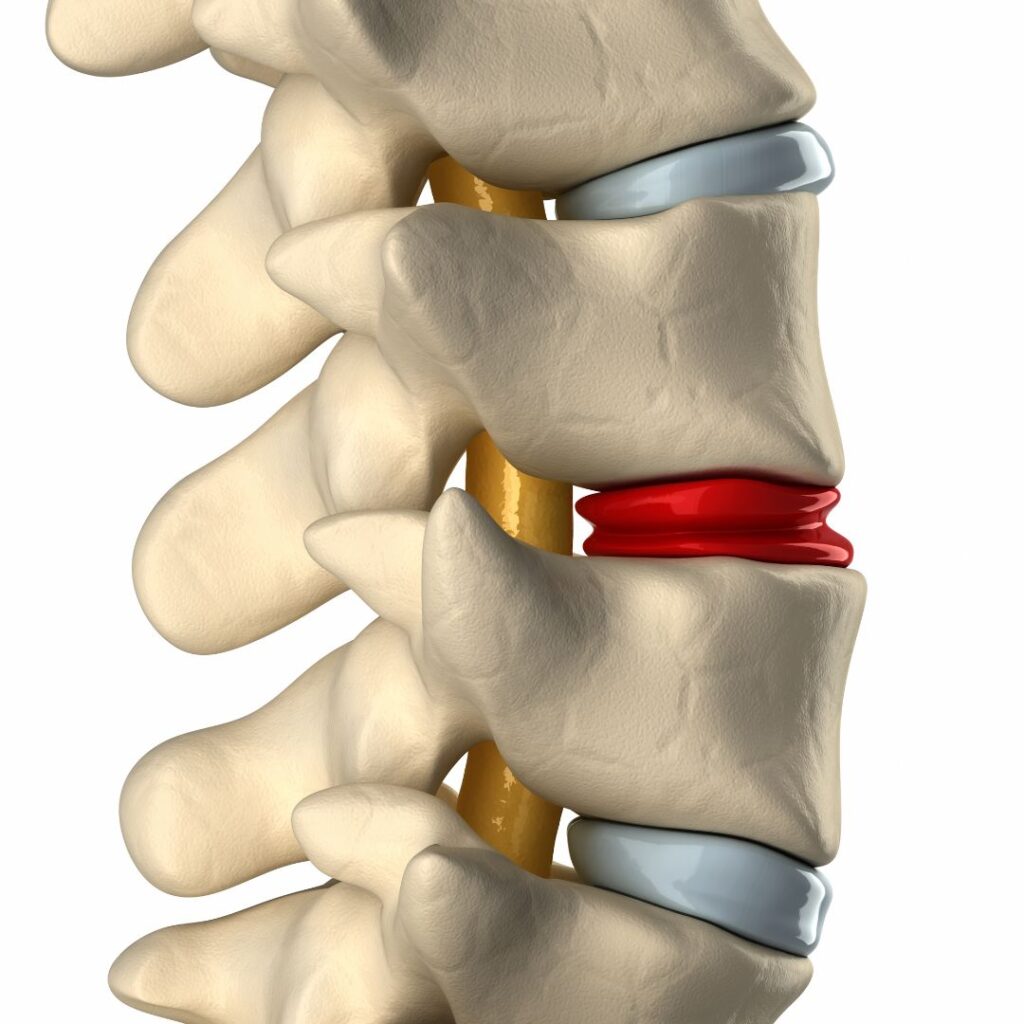
Thoracic Disc Injury:
Disc protrusions, disc herniations, or extrusion can irritate or compress a thoracic nerve
Thoracic Facet Arthritis:
Arthritis can lead to swelling within and around the joint. This can narrow the boney doorway through which the thoracic nerves exit the spine leading to thoracic radiculopathy.
Ligament Thickening:
A ligament is a thick fibrous band of connective tissue that connects bone to bone. When bulked up it can cause thoracic radiculopathy
Facet Cyst:
Cysts can extend beyond the facet joint potentially compromising the thoracic nerve.
Unstable rib attachments:
Excessive movement of the rib head at its attachment to the spine can cause nerve root irritation
Bone Spurs:
Abnormal boney growths can also irritate or compress a thoracic nerve.
Why Is Radiculopathy In The Thoracic Difficult To Diagnose?

The chest cavity contains many structures which include the thoracic spine, ribs, disc, facet joints, nerves, costovertebral joints, and ligaments in addition to vital organs. These include the heart, lungs, liver, spleen, pancreas, kidneys, and bowel. Each of these is susceptible to injury with resultant pain.
Because of the many different structures within the chest cavity oftentimes it is difficult to identify the source of a given pain. Pain arising in the thoracic spine may come from one or more sources. Is the pain due to thoracic nerve irritation or is it being referred from the lung? This is what makes the diagnosis of thoracic radiculopathy difficult.
Pain perceived in the thoracic spine is not always originating from the spine. Pain perceived or felt in an area different from the actual tissue damage is called referred pain. An example is a kidney stone. The tissue injury is within the kidney but many patients complain of the severe chest wall and flank pain.
How Specialists Check For Radiculopathy In The Thoracic
The first step in identifying thoracic radiculopathy begins with a review of current and past medical and surgical history along with a thorough physical examination.
- Numbness or lack of sensation
- Muscle reflexes: nerve irritation may cause diminished reflexes.
- Muscle endurance: when the electrical signal to a given muscle is compromised the muscle can start to shrink in size.
- Spinal posture: spinal alignment is key to the health and vitality of the thoracic spine. Abnormal curves in the spine such as kyphosis or scoliosis can cause thoracic radiculopathy.
Diagnostic tests may include:
- X-rays to evaluate the alignment of spinal bones
- Thoracic spine MRI: detailed 3D imaging of the spine evaluating the discs, facet joints, ligaments, and nerves for injury.
How To Relieve Thoracic Nerve Pain
Conservative treatments when appropriate should always be the first step in the treatment of thoracic radiculopathy. They include:
- Rest
- Stretching
- Physical Therapy
- Chiropractic Care
- Ice/Heat
- Medications: NSAID, muscle relaxants, and nerve medications like Lyrica and Cymbalta.
Why Epidural Steroids Are A Bad Idea For Your Spine

When conservative treatments fail, many patients are referred for an epidural steroid injection. The goal of an epidural steroid injection is to reduce inflammation around the nerve. Steroids are very powerful anti-inflammatory agents. Common examples include Solumedrol, betamethasone, and methylprednisolone.
The bad news is that corticosteroids are extremely toxic to local stem cells around the spine that maintain the health of the local tissue (1, 2). They also damage the cartilage in the facet and costotransverse joint.
Traditional spine physicians treat thoracic radiculopathy with high-dose corticosteroid epidurals to reduce inflammation around the nerve root.
While corticosteroids do have a potent anti-inflammatory effect when placed around the nerves, this can reduce symptoms. The bad news is that corticosteroids are extremely toxic to the local stem cells around the spine that maintain the health of local tissue (1,2).
In addition to local toxicity, they have systemic effects. Epidural steroid injections have been associated with a 29% increase in spinal fracture risk, for each epidural shot, in middle-aged and older women due to bone loss (3,4).
Another risk women assume with epidural steroid injections is vaginal bleeding after the procedure and studies show these shots can cause poor blood-sugar control in diabetics (5, 6).
Can Steroids Affect Your Hormones?
Epidural steroid injections have been shown to suppress the hypothalamus-pituitary-adrenal (HPA) axis, which is the brain loop that allows you to respond to stress and inflammation. The effect lasts as much as three weeks after just one injection.
These hormones affect the function of almost every tissue type in your body (7)! This suppression effect can create problems with energy reserves, hormonal regulation, the nervous system, and immune function, and increase susceptibility to illnesses.
A similar effect was also found with steroids injected into knees, with a resulting 60% of subjects showing adrenal problems two months after their steroid injections (8).
Steroid injections into knees are also associated with significant cartilage loss with no clinically significant improvement in pain.(9). If all of this isn’t enough, we’ve seen many studies simply showing these epidural steroid injections are providing less relief than the anesthetic alone (10).
So Why Are Steroids Always Recommended?
When conservative treatment fails, many patients are referred for an epidural steroid injection. Steroids are a readily, low-cost treatment option for patients in pain. Steroids can be taken orally, injected intravenously, or intramuscularly. Steroids are powerful anti-inflammatory agents.
Why did one steroid help, but the additional ones help minimally, if at all?
- First epidural: Knocks down the inflammatory process but also kills off the important local stem cells that maintain the tissue.
- Second epidural: Continues to reduce inflammation but again takes out the most local maintenance cells
- Third epidural: Most of the inflammation is gone but all the local cells that keep the tissue healthy are no longer present and pain starts to build because tissue continues to break down.
Can Surgery Help Thoracic Radiculopathy?
When conservative therapy and steroid epidural injections fail to provide significant or sustained benefit some patients are referred for surgical consultation.
The 3 most common thoracic surgeries were discussed in a previous blog. They include
- Posterior thoracic fusion
- Thoracic Laminectomy
- Thoracic Discectomy
The biggest problem with thoracic spine surgery is the complications. They include:
- Infection
- Bleeding
- Nerve injury
- Lung Injury/Collapse
- Rib Injury
- Increased pain
- Spinal cord injury
The complication rate is as high as 35%, and given the unique aspects of the thoracic spine, rib attachments, lungs nearby, many large blood vessels, spinal cord, and other vital structures, the complications from surgery can be severe and life-threatening.
These complications can be infections, re-herniation of the disc, persistent pain, further degeneration of the disc, and spinal cord or nerve injury. Some complications do not show up until after surgery. Some show up quickly and some may take months to become evident (11).
More Treatment Options
Cervical Epidural Steroid Injection
The neck pain started out as a dull ache but steadily progressed. It becomes constant and oftentimes keeps you up at night. Turning your head can send an electrical current down your arm. Rest, medications and physical therapy failed to provide much relief. Your doctor referred you to a pain clinic for a Cervical Epidural steroid injection. The injection was performed at an ambulatory surgical center. Unfortunately, the pain is now worse. What is a Cervical Epidural injection? Are there different types of Cervical Epidural injections? What are…
Read More About Cervical Epidural Steroid InjectionDisc Replacement Surgery
The surgeon first accesses the spinal column (for example, in the cervical spine, the surgeon would access the spine through an incision in the front of the neck). From here the surgery is quite aggressive as the disc is scraped and chiseled out of the disc space. Pins are screwed into the vertebrae above and below the disc space that will anchor the space in place as the surgeon works. A tool is inserted into the disc space and used to further separate the upper and lower vertebrae, enlarging the space. The vertebrae surfaces within the disc space are prepared…
Read More About Disc Replacement SurgeryNerve Hydrodissection
Nerve Hydrodissection is a medical procedure that aims to free up scar tissue or adhesions on a given peripheral nerve. The procedure utilizes ultrasound guidance to visualize both the needle and the targeted nerve. Medication is then injected through the needle to free up the scar tissue. Nerve Hydrodissection is a minimally invasive treatment option for many peripheral nerves that are compressed or entrapped by scar tissue.Pain is an uncomfortable and at times painful sensation. It varies significantly from patient to patient. There are many different types of pain which include inflammatory, nociceptive, and neuropathic. Neuropathic pain is pain that arises from nerve compression or injury.
Read More About Nerve HydrodissectionNeuro-Prolotherapy (Neural-Prolo)
Neural-Prolo, is also known as Neurofascial Prolotherapy (NPT). Born from traditional prolo-therapy, Neural-Prolo is described as: Subcutaneous peri-neural injection of 5% dextrose. It was created by a New Zealand physician, Dr. John Lyftogt while he was treating a series of Achilles tendon injuries. Similar to how traditional prolotherapy helps strengthen loose ligaments and damaged tendons, Dr. Lyftogt discovered that a low concentration of dextrose (5%) in the subcutaneous tissue can help in resolving chronic nerve inflammation and restoring the normal physiology of the nerve cell. Neuritis is also thought to be a contributing factor to chronic pain syndromes and why sometimes the pain continues…
Read More About Neuro-Prolotherapy (Neural-Prolo)NSAIDs
The other day I was evaluating a patient and reviewing the treatment options for their spine condition. After discussing prior treatments, we got to the topic of medications taken for pain relief. She explained that she mainly utilized anti-inflammatory (NSAID) medications and then she told me to hold much she takes and has been for many years…..she takes close to 2 grams (2000 milligrams) on a daily basis which equated to about 9-10 capsules of medication per day. I was shocked, considering she was pre-diabetic and with high blood pressure plus the kicker of it is that her PCP (primary care physician) is ok with this…
Read More About NSAIDsPerc-FSU – Trusted Alternative to Spinal Fusion
The Perc-FSU Procedure is an injection-based treatment that utilizes the patients’ own blood platelets to bring stability to the spine without the need for the rods, nuts, bolts, and hardware of fusion surgery. “Perc” stands for percutaneous, and “FSU” stands for “Functional Spinal Unit,” which means that the spine is treated as one functioning unit. Up and down the spine, the discs, facet joints, ligaments, and muscles that assist in stabilizing the spine are treated with image-guided injections of PRP and Platelet Lysate to help bring stability to the spine as a whole. It is the trusted alternative to spinal fusion.
Read More About Perc-FSU – Trusted Alternative to Spinal FusionProlotherapy For Thoracic Pain
Prolotherapy is an injection based regenerative therapy used in the treatment of ligament, tendon, muscle and spine injuries. It is minimally invasive and involves the injection of an irritant such as dextrose into the damaged or painful area. The injected irritant stimulates a delayed or frozen healing cycle thereby increasing blood flow and tissue healing. The thoracic spine is that section of the spine that is below the neck and above the low back. It is also referred to as the mid back. It has multiple components that include: Vertebral Bodies: Boney building blocks that stack one upon another…
Read More About Prolotherapy For Thoracic PainProlotherapy Injections
It has been successful in the treatment of many disorders including neck, shoulder, knee, and ankle pain. Dr. Centeno recently published an article in The Journal of Prolotherapy in which he discusses the use of x-ray guidance with prolotherapy. This ensures that the injection is in the correct place to maximize clinical results. Dr. Centeno discusses the use of prolotherapy for the treatment of neck, knee, sacroiliac joint, ankle, ischial tuberosity, and shoulder pain. At the Centeno-Schultz Clinic x-ray guided prolotherapy is just one of the therapies utilized in the successful treatment of pain. Regenerative injection therapy (RIT) or prolotherapy…
Read More About Prolotherapy InjectionsPRP for Nerve Damage
Peripheral nerves are comprised of various combinations of motor, sensory, and autonomic neurons. Nerve injuries are a common condition with a broad range of symptoms depending on the severity of nerve damage which presents various challenges to patients, ranging from mild discomfort to life-long impairment. PRP for nerve damage has been shown to be effective. Let’s dig in. Nerve injuries can be classified based on the severity of damage and which structures in the nerve have been damaged. The most severe case is the complete transection of the nerve, called neurotmesis. The most common is neuropraxia from acute or chronic compression of the nerve.
Read More About PRP for Nerve DamagePRP Injections
PRP is short for platelet-rich plasma, and it is autologous blood with concentrations of platelets above baseline values. The potential benefit of platelet-rich plasma has received considerable interest due to the appeal of a simple, safe, and minimally invasive method of applying growth factors. PRP treatments are a form of regenerative medicine that utilizes the blood healing factors to help the body repair itself by means of injecting PRP into the damaged tissue. In regenerative orthopedics, it is typically used for the treatment of muscle strains, tears, ligament and tendon tears, minor arthritis, and joint instability. There have been more than 30 randomized controlled trials of PRP…
Read More About PRP InjectionsAlternatives To Traditional Medical Treatments
Is there an alternative to corticosteroids that can help prevent the need for surgery?
In 2017, we published the world’s first clinical research article outlining a better way to treat radiculopathy compared to steroid injections. We have been utilizing these advanced injections for the past 15 years and seeing excellent results.
Platelet-Rich Plasma Injections
Here is a quick video outlining the use of platelet-rich plasma called platelet lysate in spine treatment.
Seek A Better Solution For Thoracic Radiculopathy

We have been treating thoracic radiculopathies for over a decade with excellent results that are safer and more effective when compared to traditional corticosteroid epidurals.
If you have been diagnosed or have symptoms that fit this diagnosis, feel free to contact our office to get set up for an evaluation where we can further discuss these treatment options and discuss your candidacy for these procedures.
Thoracic radiculopathy shouldn’t keep you from living the life you want. Schedule an appointment with us today
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate and PRP for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI).
More Resources for Thoracic Conditions
The Spine Owner’s Manual: How to Avoid Back Pain & Life-Altering Surgery
This e-book from Dr. Chris Centeno focuses on the spine and how it functions within the human musculoskeletal system and the body as a whole. Everything in our bodies works together like a well-tuned symphony to support our well-being, and a strong spine (including all of its component parts, such as spinal nerves, ligaments, muscles, etc.) is critical to complete health.
Using the Regenexx SANS approach, The Spine Owner’s Manual provides a series of tests and clearly defined exercises that you can do on your own to measure and monitor your own spinal health. These musculoskeletal tests will allow you to monitor where your own body might be struggling to maintain proper stability, articulation, symmetry, and neuromuscular function.
-
Understanding the Thoracic and Lumbar Spines
The thoracic spine and lumbar spine make up a vital nexus of stability and mobility in the human body. In this exploration, we delve into the biomechanics and complexities that define these regions, unraveling their significance in posture, movement, and overall well-being. Understanding the thoracic and lumbar spine not only illustrates the mechanics of our…
-
Understanding the Role Of The Thoracic Spine Muscles
The thoracic spine plays a critical role in the stability and mobility of the upper body. Comprised of twelve vertebrae and an intricate network of muscles and ligaments, it serves as a central pillar supporting the structure and movement of the body. Understanding the role and function of thoracic spine muscles is pivotal for anyone…
-
Degenerative Changes Of The Thoracic Spine
Degenerative changes of the thoracic spine involve the gradual loss of normal structure and function over time. There are several different causes which are discussed in detail below. The thoracic spine is composed of many different and important components that are susceptible, both to injury and generalized wear and tear. The degeneration can occur in…
-
The Ultimate Guide To Thoracic Spine Exercises
Thoracic spine exercises are important for several reasons. First, they can help improve thoracic mobility, reducing the risk of spinal injuries and improving posture. Second, they can help to strengthen the muscles of the upper back and shoulders. Finally, thoracic spine exercises can help improve breathing mechanics. What Is Thoracic Spine? The thoracic spine, also…
-
Where Is The Thoracic Spine?
The thoracic spine is a region of the spine that is located in the middle back. It is located below the cervical spine and above the lumbar spine. It is composed of 12 vertebrae that are numbered T1-12. The T denotes the thoracic spine. It has many important functions which are discussed below. Location Of The…
-
Symptoms of Thoracic Herniated Disc
Your mid back pain has been unrelenting since the accident. Rest, medications, and physical therapy have failed to provide significant or sustained benefits. Your doctor thinks you have a thoracic disc herniation and thinks you have a thoracic herniated disc. What are the symptoms? And what can you do? Let’s dig in. What Is A…
References
1.Zhang AZ, Ficklscherer A, Gülecyüz MF, et al. Cell Toxicity in Fibroblasts, Tenocytes, and Human Mesenchymal Stem Cells-A Comparison of Necrosis and Apoptosis-Inducing Ability in Ropivacaine, Bupivacaine, and Triamcinolone. Arthroscopy. 2017;33(4):840-8. https://www.ncbi.nlm.nih.gov/pubmed/28089496
2. Wyles CC, Houdek MT, Wyles SP, et al. Differential cytotoxicity of corticosteroids on human mesenchymal stem cells. Clin Orthop Relat Res. 2015;473(3):1155-64. https://www.ncbi.nlm.nih.gov/pubmed/25187334
3. Carreon LY, Ong KL, Lau E, et al. Risk of Osteoporotic Fracture After Steroid Injections in Patients With Medicare. Am J Orthop. 1976;46(5):E293-E300. https://www.ncbi.nlm.nih.gov/pubmed/29099886
4.Nah SY, Lee JH, Lee JH, et al. Effects of Epidural Steroid Injections on Bone Mineral Density and Bone Turnover Markers in Patients Taking Anti-Osteoporotic Medications. Pain Physician. 2018;21(4):E435-E447. https://www.ncbi.nlm.nih.gov/pubmed/30045610
5. Even JL, Crosby CG, Song Y, et al. Effects of epidural steroid injections on blood glucose levels in patients with diabetes mellitus. Spine. 2012;37(1):E46-50. https://www.ncbi.nlm.nih.gov/pubmed/21540770
6. Shanthanna H, Busse JW, Goudsmit EM, et al. Abnormal vaginal bleeding after epidural steroid injection: is there a cause for concern. Evid Based Med. 2014;19(2):e16. https://www.ncbi.nlm.nih.gov/pubmed/24282169
7. Habib G, Jabbour A, Salman J, et al. The effect of epidural methylprednisolone acetate injection on the hypothalamic-pituitary-adrenal axis. J Clin Anesth. 2013;25(8):629-33. https://www.ncbi.nlm.nih.gov/pubmed/23988802
8. Johnston PC, Lansang MC, Chatterjee S, et al. Intra-articular glucocorticoid injections and their effect on hypothalamic-pituitary-adrenal (HPA)-axis function. Endocrine. 2015;48(2):410-6. https://www.ncbi.nlm.nih.gov/pubmed/25182149
9. McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA. 2017;317(19):1967-75. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5815012/
10. Felson DT, Anderson JJ, Goudsmit EM, et al. Across-study evaluation of association between steroid dose and bolus steroids and avascular necrosis of bone. Lancet. 1987;1(8538):902-6. https://www.ncbi.nlm.nih.gov/pubmed/2882300
11. Manchikanti L, Knezevic NN, Boswell MV, et al. Epidural Injections for Lumbar Radiculopathy and Spinal Stenosis: A Comparative Systematic Review and Meta-Analysis. Pain Physician. 2016;19(3):E365-410. https://www.ncbi.nlm.nih.gov/pubmed/27008296
12. McCormick WE, Will SF, Benzel EC. Surgery for thoracic disc disease. Complication avoidance: overview and management. Neurosurg Focus. 2000;9(4):e13. https://www.ncbi.nlm.nih.gov/pubmed/29225115
13. O’Connor RC, Andary MT, Russo RB, et al. Thoracic radiculopathy. Phys Med Rehabil Clin N Am. 2002;13(3):623-44, viii. https://www.ncbi.nlm.nih.gov/pubmed/12380552