You might not be able to imagine your doctor as a patient, but doctors sometimes find themselves on the other side of the stethoscope. Our own Dr. Centeno is a good example of a doctor turned patient when it comes to diagnosing and treating degenerative spondylolisthesis. A degenerative condition, without intervention, will only worsen over time, and this is why diagnosing degenerative spondylolisthesis early, as Dr. Centeno knows as both a doctor and a patient, is so critical.
The Doctor Becomes the Patient
During residency training, Dr. Centeno broke three transverse processes (bone projections on the sides of each spine vertebra) in an accident in which he flipped his Jeep. As a result, he has S1 radiculopathy (irritation of the S1 spinal nerves) with intermittent back pain. This hasn’t limited him much; though he doesn’t run anymore, he is very active and lifts heavy weights. He’s kept his back issue under control by becoming the patient of another physician and being treated here at the clinic a couple of times a year. During a recent exam, however, his physician noticed that his L5 vertebra was starting to slip forward, adding a more urgent level of concern to his back issue. Let us explain.
Defining Degenerative Spondylolisthesis
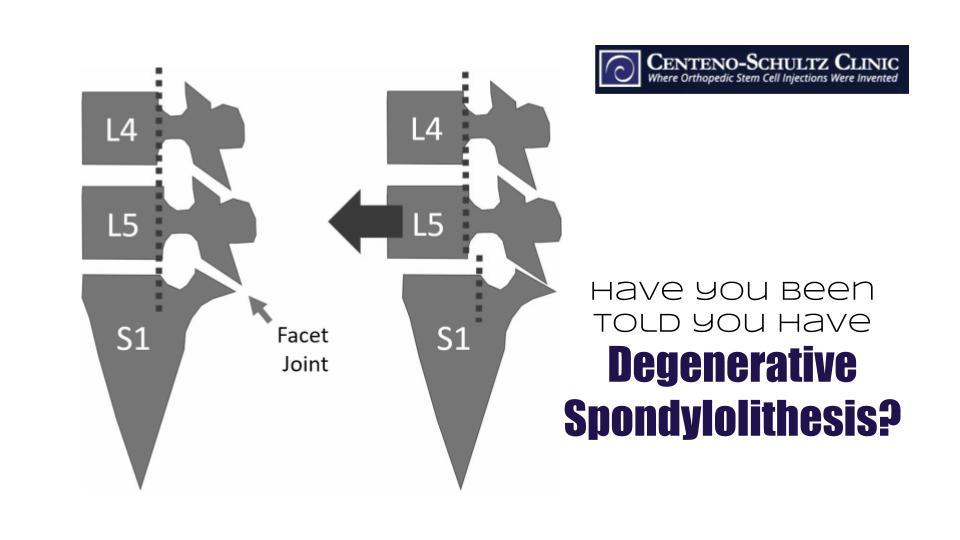
The bones of the spine (vertebrae) are stacked one on top of the other (see image below). Spondylolisthesis occurs when one bone slips forward on the other. While this issue can be present at birth due to when the bones are simply formed without the proper connections, it can also occur with degenerative wear and tear. In the latter case, this is called degenerative spondylolisthesis.

The Progression of Degenerative Spondylolisthesis
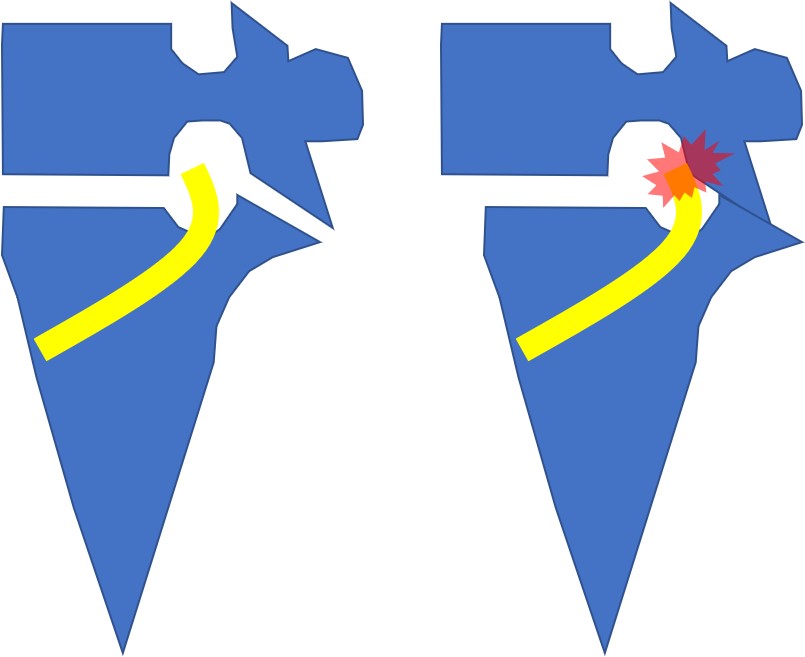
The nerves that supply your lower limbs and transmit signals from there to the brain pass through the foramen in the spinal column. The foramen is an opening (shown in the image below with the yellow representing a nerve exiting the foramen), between two vertebrae. The image on the left shows a normal foramen and nerve; compare this to the image on the right, which shows what happens when a vertebra slips forward. The opening is restricted and the nerve becomes pinched. If the facet joint has arthritis, inflammation can add to the pressure and restrict the space further. In addition, the disc between the affected back bones can be damaged (e.g., bulging or herniated disc), creating even more pressure and irritation on the nerve.
Treating Degenerative Spondylolisthesis
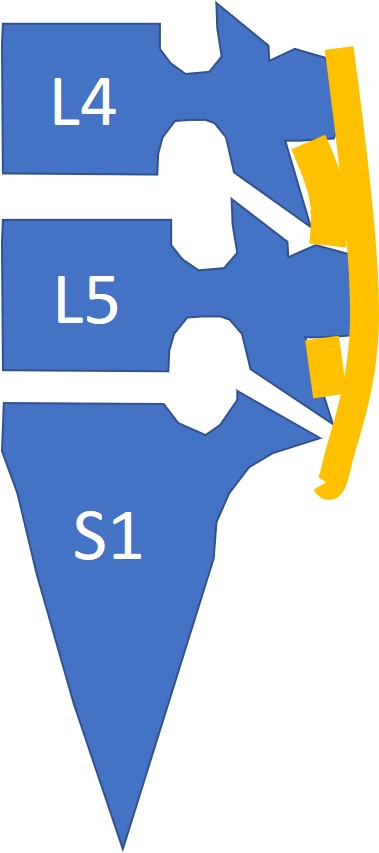
Note in the image below that there are ligaments (supraspinous and interspinous ligaments) that are positioned at the back of the spine (shown in orange). With the help of the iliolumbar ligaments, they provide resistance to forward movement. So loose ligaments also contribute to degenerative spondylolisthesis.
Dr. Centeno opted to have his degenerative spondylolisthesis treated with a percutaneous ligamentoplasty with platelets once a month for several months. Why so many? Because if the vertebra continues to move farther forward, the facet joint will become more damaged and harder and harder to treat nonsurgically. Hence, the aggressive treatment.
Both diagnosing and treating degenerative spondylolisthesis early are critical to lowering the risk of surgery, such as decompression or fusion. Addressing the loose spinal ligaments is key, and Dr. Centeno can speak to this not only as a treating physician but also as a degenerative spondylolisthesis patient.