Your mid back pain has been unrelenting since the accident. Rest, medications, and physical therapy have failed to provide significant or sustained benefits. Your doctor thinks you have a thoracic disc herniation and wants to refer you to a surgeon. Is surgery your best option for a thoracic herniated disc? What are the different types of thoracic disc surgeries? What are the risks, complications, success, and recovery times of each type of surgery? What are the non-surgical treatment options? Is PRP effective for the treatment of herniated thoracic discs? Why is getting a proper diagnosis so important? Let’s dig in.
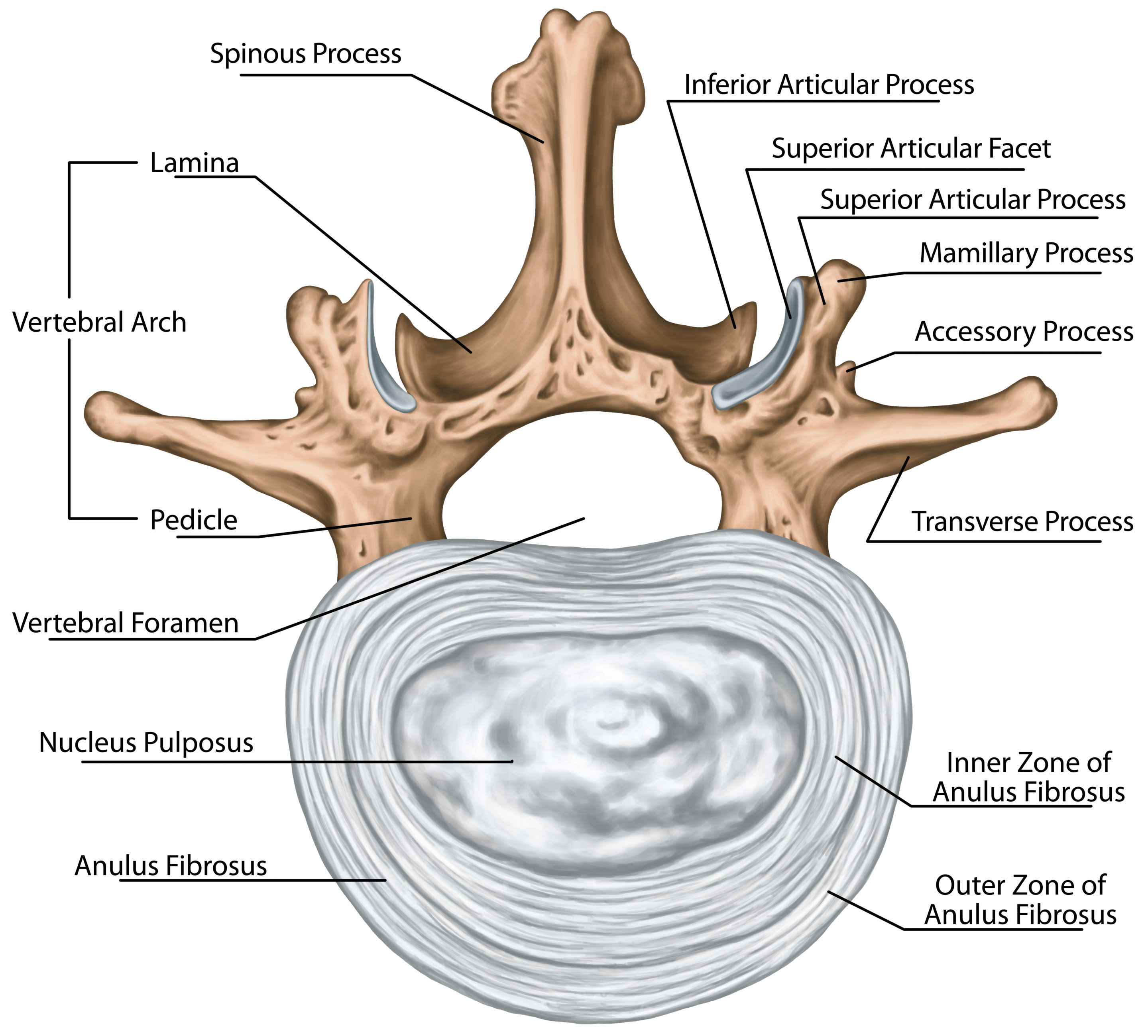
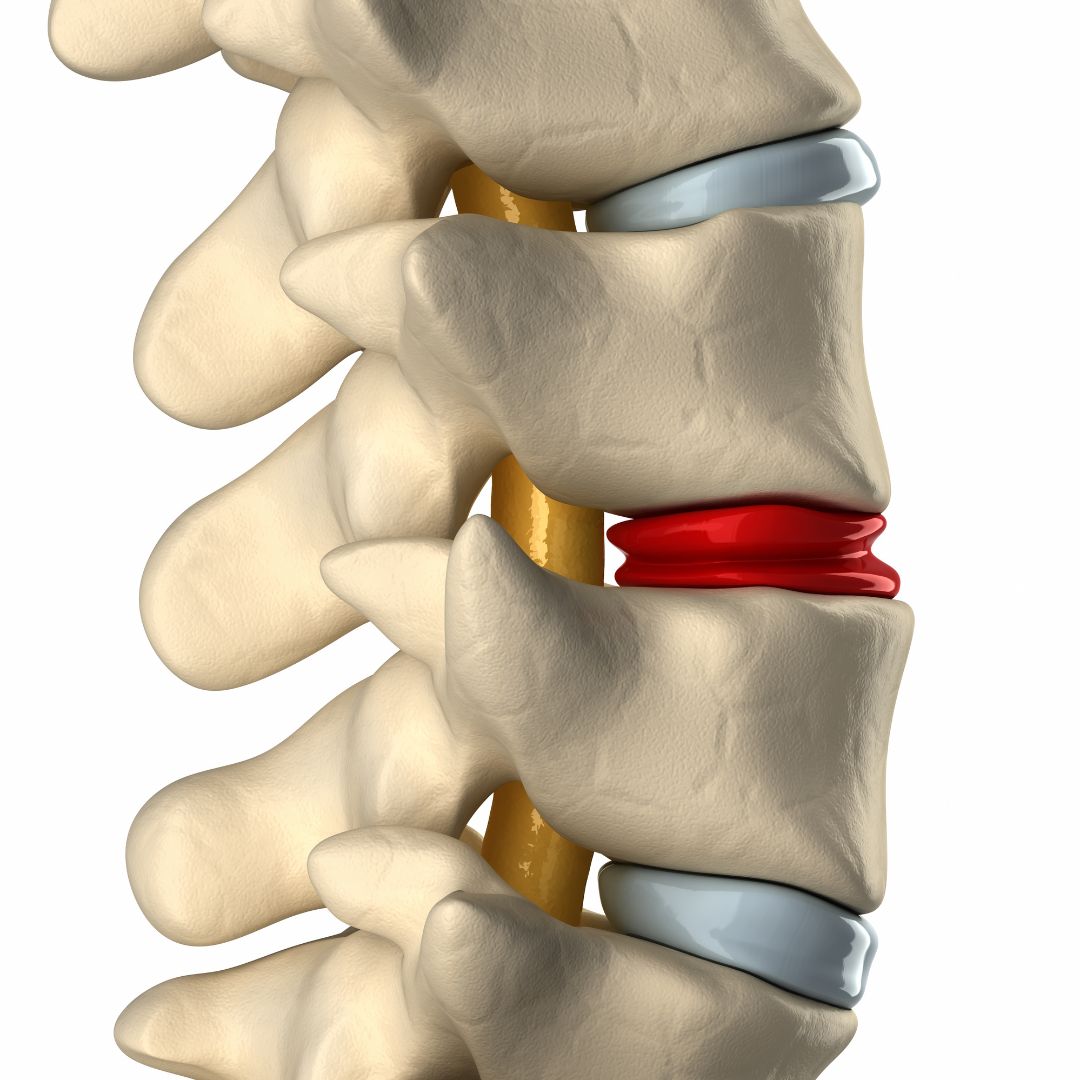
Disc herniation is a painful medical condition in which the central portion of the disc is pushed outside of the disc and into the spinal canal. This occurs due to a weakness or injury to the outer sidewall of the disc. Pain, muscle spasm, muscle weakness, and numbness can occur. It can occur in the neck, low back, and thoracic spine. When conservative treatments fail, patients are often referred for thoracic herniated disc surgery.
Types Of Thoracic Herniated Disc Surgeries
The goal of thoracic herniated disc surgery is to remove that portion of the herniated disc that is responsible for the ongoing pain and compression of the nerves. The disc can herniate in a number of different directions. Examples include central disc herniation vs right or left-sided thoracic disc herniations. The orientation of the disc herniation is important as it can play a role in the type of thoracic disc surgery recommended. Another important factor is the size of the thoracic disc herniation and what structures are being compressed.
Thoracic herniated disc surgery is much more complicated than surgery for cervical or lumbar herniations. Why? The thoracic cavity contains many more vital structures, including the spine, exiting nerves, ribs, heart, lungs, liver, pancreas, and bowel. The working space around a thoracic herniated disc is much smaller and all the adjacent structures including the exiting nerves and lungs are susceptible to injury. Thoracic herniated disc surgery is complex due to the limited working space, a large number of adjacent tissues, and the risk of permanent, life-changing injuries.
Thoracic Laminotomy / Laminectomy
A thoracic laminectomy is a major surgery in which a part of the spinal bone is removed so as to reduce the pressure on the spinal cord and nerve roots (1). The lamina is the ” roof of the spinal canal that provides support and protection for the spinal cord. It is located on the backside of the thoracic spine. A thoracic disc herniation can compress the spinal cord and nerves. A thoracic laminectomy removes the roof of the spinal canal and in so doing decreases the pressure and potential damage to the spinal cord and nerves.
A laminotomy involves partial removal of the laminae whereas a laminectomy involves complete removal of the lamina. Both procedures are performed using a posterior (backside) approach.
Risks Associated with Thoracic Laminotomy/Laminectomy
Thoracic laminotomy and laminectomy are both complex surgeries with significant risks and complications. The major risks include infection, failure, escalation in pain, and injury to eh spinal cord, nerve root, dura, ribs, and lungs. Removal of all or a portion of the lamina and surrounding ligaments can lead to thoracic spine instability.
Success Rate & Research Relating to a Thoracic Laminectomy
A systematic review and meta-analysis of six studies demonstrated the following complications (2):
Dural tears occurred in all six studies (3).
Cerebral spinal fluid leaks occurred in 5 studies (4).
Infection occurred in three studies with an incidence of 4.8% (5).
Success rates vary depending on the size of the thoracic disc herniation, the severity of the spinal cord and nerve compression, the surgical approach, and the number of levels treated. Minimally invasive techniques are currently being evaluated.
Recovery Time After a Thoracic Laminotomy/Laminectomy
Recovery rates vary and can take months to recover. The time required to recover from laminotomy ( partial removal of lamina) is considerably shorter than the laminectomy (full removal of lamina)( 6).

Life After A Thoracic Laminotomy/Laminectomy
Resolution of pain and dysfunction is not guaranteed with thoracic laminotomy/ laminectomy. Pain may remain the same or may increase after surgery. Post-surgery patients may have new symptoms due to irritation or injury of the adjacent structures which include the ribs, exiting nerves, and the spinal cord covering (dura). Cutting essential muscles and ligaments can lead to thoracic instability and abnormal forward posture (kyphosis) (7). Life after thoracic laminotomy/laminectomy may involve stiffness, muscle tightness, and a restricted range of motion.
Thoracic Discectomy
A discectomy is a surgery that involves the removal of the damaged part of the disc. It can be performed at all levels of the spine; cervical, thoracic, and lumbar. The goal of a posterior thoracic discectomy is to remove that portion of the disc that is injured and causing pain. In addition, a thoracic discectomy removes that portion of a disc causing irritation or damage to the spinal cord or nerves. In theory, removing the damaged disc will improve pain and relieve pressure on the neural elements such as the spinal cord.
A disc may herniate in a number of different directions including to the right or left, posteriorly into the spinal canal, or anteriorly. This will dictate the surgical approach that is used. Anterior refers to the front whereas posterior is the back. A posterior thoracic discectomy requires significant cutting of the muscles and ligaments which can destabilize the thoracic spine. An anterior approach, on the other hand, requires the assistance cardiovascular surgeon as the lungs must be moved out of the way to expose the thoracic herniated disc. Often times ribs are broken or cut. Ouch!
Risks Associated with Thoracic Discectomy
Risks associated with thoracic discectomy include dural tears, nerve injury, spinal cord injury, vascular complication, infection, escalation in pain, continued degeneration of the affected disc, intercostal neuralgia, and failure. In addition, disc degeneration may be accelerated by the discectomy (8).
Success Rate & Research Relating to a Thoracic Discectomy
The size of the thoracic disc herniation and the presence of any calcification are both predictors of poor outcomes (9). Success rates vary significantly based upon the indication for the thoracic discectomy, levels performed, presence or absence of fusion, and pre-existing medical conditions. In one study at 37 months, post-surgery only 40% of patients reported excellent results (10). In the same study at 3-6 months, only 60% reported improved motor function.
Recovery Time After a Thoracic Discectomy
Recovery time after thoracic discectomy varies and is dependent upon the patient’s age, current medical conditions, size of the disc herniation, amount of muscle, tendon, ligament, bone resected, and injury to the spinal cord, and exiting nerves. Extensive physical therapy is required. It takes 3-6 months for most patients to report any clinical improvement.
Life After A Thoracic Discectomy
Thoracic discectomy is a major surgery. Life after thoracic discectomy may improve depending upon a number of factors. Life may also significantly change along with the quality of life due to potentially permanent complications. These include nerve damage, spinal cord injury, acceleration of disc degeneration, thoracic facet damage, and injury to the lungs.
Conclusion
Thoracic herniated disc surgery because of its invasive nature and significant and potentially permanent complications should be reserved for cases of bowel and bladder dysfunction, progressive lower extremity weakness, and severe pain that does not get better after conservative care.
Can A Thoracic Herniated Disc Heal Without Surgery?
Yes! A thoracic herniated disc can heal without surgery. Many respond to conservative care. When appropriate, conservative care should be the first treatment of choice. Conservative treatment options are discussed below. Thoracic disc herniation surgery should be the treatment of last resort given the significant and potentially permanent complications. Surgery does not guarantee a reduction in pain and may in fact aggravate the pain.
The Centeno-Schultz Clinic are experts in the evaluation and treatment of thoracic disc herniations. It starts with a comprehensive evaluation where current and past medical history, medications, past surgeries, and traumas are reviewed. Imaging is reviewed which may include x-rays, MRI, and CT scans. In-office ultrasounds are invaluable as they provide a life snapshot of the muscles, tendons, ligaments, nerves, and bones in the thoracic cavity. Treatment options include x-ray and ultrasound-guided injection of PRP and bone marrow concentrate.
To learn more about the symptoms and causes of disc herniation in the thoracic spine, read our article “Symptoms of Thoracic Herniated Disc“
Non-Surgical Interventional Treatments
Given the significant and potentially permanent compilations associated with thoracic disc herniation surgery, it is important to consider conservative treatment options. Examples include:
- Rest
- Stretching
- Physical Therapy
- Ice/Heat
- Trial of NSAID
- Chiropractic Care
PRP For Thoracic Disc Herniation
Disc degeneration is a common cause of thoracic disc herniations. Disc degeneration is the cumulative affect of wear and tear on the spine. Blood flow to the spine provides oxygen and other important nutrients to the disc. Blood flow to the spine is like water to a garden. Unfortunately, the thoracic discs have poor blood flow.
At the Centeno-Schultz Clinic PRP injections are one of the treatment options for thoracic disc herniations. Injections are performed under x-ray and ultrasound guidance. Why? To avoid puncture and collapse of a lung.
Why PRP? PRP contains may different growth factors. A specific one called VEGF can potentially increase blood flow to a given area. Increased blood flow can potentially accelerate healing and tissue repair.
To learn more about PRP at the Centeno-Schultz Clinc, please click here.
Unlike traditional pain clinic, the Centeno-Schultz Clinic focuses on the spine and all its parts as a whole. The many different parts of the thoracic spine do not work in isolation. Rahter they work together in a highly synchronized way. The approach is referred to a functional spinal unit. A very specific and comprehensive approach to the spine is utilized in the treatment of many thoracic injuries. This is referred to as the Regenexx Perc-FSU.
Get A Proper Diagnosis To Come Up With The Most Appropriate Treatment Plan
Thoracic disc herniation is a painful medical condition in which the central portion of the disc is pushed outside of the disc and into the spinal canal. When appropriate, conservative treatments option should be the treatment of choice. Thoracic laminectomy is a surgical treatment option in which a portion of the spinal bone is removed to relieve the pressure on the spinal cord and nerves. Thoracic discectomy is a surgery that removes the damaged, painful part of the disc. Both are associated with significant and potentially permanent complications. Recovery for both surgeries is extensive and takes months of dedicated, often painful therapy. There are no guarantees with surgery. The pain and dysfunction may not improve. Permanent life-altering complications can occur.
A proper and accurate diagnosis is the first step in the effective treatment of throacic spine and disc injuries. This requires a dedicated team to evaluate all possible pain sources. Conservative and regenerative treatment options would be exhausted prior to considering thoracic disc herniation surgery. At the Centeno-Schultz Clinic we are committed to a thorough evaluation and proper diagnosis. Only then can treatment options be discussed.
Are you unsure about getting surgery for your thoracic spine condition? To schedule please contact Jen at 720-287-7196 or [email protected] or Vanessa at [email protected]. It is time to stop suffering and start living life to its fullest.
John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate and PRP for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI).
The Spine Owner’s Manual: How to Avoid Back Pain & Life-Altering Surgery
This e-book from Dr. Chris Centeno focuses on the spine and how it functions within the human musculoskeletal system and the body as a whole. Everything in our bodies works together like a well-tuned symphony to support our well-being, and a strong spine (including all of its component parts, such as spinal nerves, ligaments, muscles, etc.) is critical to complete health.
Using the Regenexx SANS approach, The Spine Owner’s Manual provides a series of tests and clearly defined exercises that you can do on your own to measure and monitor your own spinal health. These musculoskeletal tests will allow you to monitor where your own body might be struggling to maintain proper stability, articulation, symmetry, and neuromuscular function.
Related Blog Posts
-
Understanding the Thoracic and Lumbar Spines
The thoracic spine and lumbar spine make up a vital nexus of stability and mobility in the human body. In this exploration, we delve into the biomechanics and complexities that define these regions, unraveling their significance in posture, movement, and overall well-being. Understanding the thoracic and lumbar spine not only illustrates the mechanics of our…
-
Understanding the Role Of The Thoracic Spine Muscles
The thoracic spine plays a critical role in the stability and mobility of the upper body. Comprised of twelve vertebrae and an intricate network of muscles and ligaments, it serves as a central pillar supporting the structure and movement of the body. Understanding the role and function of thoracic spine muscles is pivotal for anyone…
-
Degenerative Changes Of The Thoracic Spine
Degenerative changes of the thoracic spine involve the gradual loss of normal structure and function over time. There are several different causes which are discussed in detail below. The thoracic spine is composed of many different and important components that are susceptible, both to injury and generalized wear and tear. The degeneration can occur in…
-
The Ultimate Guide To Thoracic Spine Exercises
Thoracic spine exercises are important for several reasons. First, they can help improve thoracic mobility, reducing the risk of spinal injuries and improving posture. Second, they can help to strengthen the muscles of the upper back and shoulders. Finally, thoracic spine exercises can help improve breathing mechanics. What Is Thoracic Spine? The thoracic spine, also…
-
Where Is The Thoracic Spine?
The thoracic spine is a region of the spine that is located in the middle back. It is located below the cervical spine and above the lumbar spine. It is composed of 12 vertebrae that are numbered T1-12. The T denotes the thoracic spine. It has many important functions which are discussed below. Location Of The…
-
Symptoms of Thoracic Herniated Disc
Your mid back pain has been unrelenting since the accident. Rest, medications, and physical therapy have failed to provide significant or sustained benefits. Your doctor thinks you have a thoracic disc herniation and thinks you have a thoracic herniated disc. What are the symptoms? And what can you do? Let’s dig in. What Is A…
1. Wang, ZW., Wang, Z., Zhou, YH. et al. Clinical effect analysis of laminectomy alone and laminectomy with instrumentation in the treatment of TOLF. BMC Musculoskelet Disord 22, 667 (2021). https://doi.org/10.1186/s12891-021-04564-3.
2.Osman NS, Cheung ZB, Hussain AK, Phan K, Arvind V, Vig KS, Vargas L, Kim JS, Cho SK. Outcomes and Complications Following Laminectomy Alone for Thoracic Myelopathy due to Ossified Ligamentum Flavum: A Systematic Review and Meta-Analysis. Spine (Phila Pa 1976). 2018 Jul 15;43(14):E842-E848. doi: 10.1097/BRS.0000000000002563. PMID: 29940604; PMCID: PMC6252088.
3. Li M, Wang Z, Du J, Luo Z, Wang Z. Thoracic myelopathy caused by ossification of the ligamentum flavum: a retrospective study in Chinese patients. J Spinal Disord Tech. 2013 Feb;26(1):E35-40. doi: 10.1097/BSD.0b013e31827ada68. PMID: 23168394.
4.Hur H, Lee JK, Lee JH, Kim JH, Kim SH. Thoracic myelopathy caused by ossification of the ligamentum flavum. J Korean Neurosurg Soc. 2009 Sep;46(3):189-94. doi: 10.3340/jkns.2009.46.3.189. Epub 2009 Sep 30. PMID: 19844616; PMCID: PMC2764014.
5.Liao CC, Chen TY, Jung SM, Chen LR. Surgical experience with symptomatic thoracic ossification of the ligamentum flavum. J Neurosurg Spine. 2005 Jan;2(1):34-9. doi: 10.3171/spi.2005.2.1.0034. PMID: 15658124.
6.Abbott R, Feldstein N, Wisoff JH, Epstein FJ. Osteoplastic laminotomy in children. Pediatr Neurosurg. 1992;18(3):153-6. doi: 10.1159/000120656. PMID: 1457375.
7. Sani, Sepehr MD*; Ratliff, John K. MD*; Cooper, Paul R. MD†. A Critical Review of Cervical Laminoplasty. Neurosurgery Quarterly 14(1):p 5-16, March 2004.
8. Kambin P, Cohen LF, Brooks M, Schaffer JL. Development of degenerative spondylosis of the lumbar spine after partial discectomy. Comparison of laminotomy, discectomy, and posterolateral discectomy. Spine (Phila Pa 1976). 1995 Mar 1;20(5):599-607. doi: 10.1097/00007632-199503010-00018. PMID: 7604330.
9.Court C, Mansour E, Bouthors C. Thoracic disc herniation: Surgical treatment. Orthop Traumatol Surg Res. 2018 Feb;104(1S):S31-S40. doi: 10.1016/j.otsr.2017.04.022. Epub 2017 Dec 7. PMID: 29225115.
10. Yang X, Liu X, Zheng Y. Surgical treatment of thoracic disc herniations using a modified transfacet approach. Indian J Orthop. 2014 Mar;48(2):158-62. doi: 10.4103/0019-5413.128756. PMID: 24741137; PMCID: PMC3977371.
Am I a Candidate?
To answer this question, fill out the candidate form below to request a new patient evaluation, and a patient advocate will reach out to you to determine your next steps. Your one-hour, in-office or telemedicine evaluation will be with one of the world’s experts in the field of Interventional Orthopedics.